Achieving Immune Harmony: A Guide to a Balanced Defense System
Achieve immune system balance. Uncover the science behind true immunity, debunk myths, and support your defenses for harmony.

Why Your Immune System Needs Balance, Not a Boost
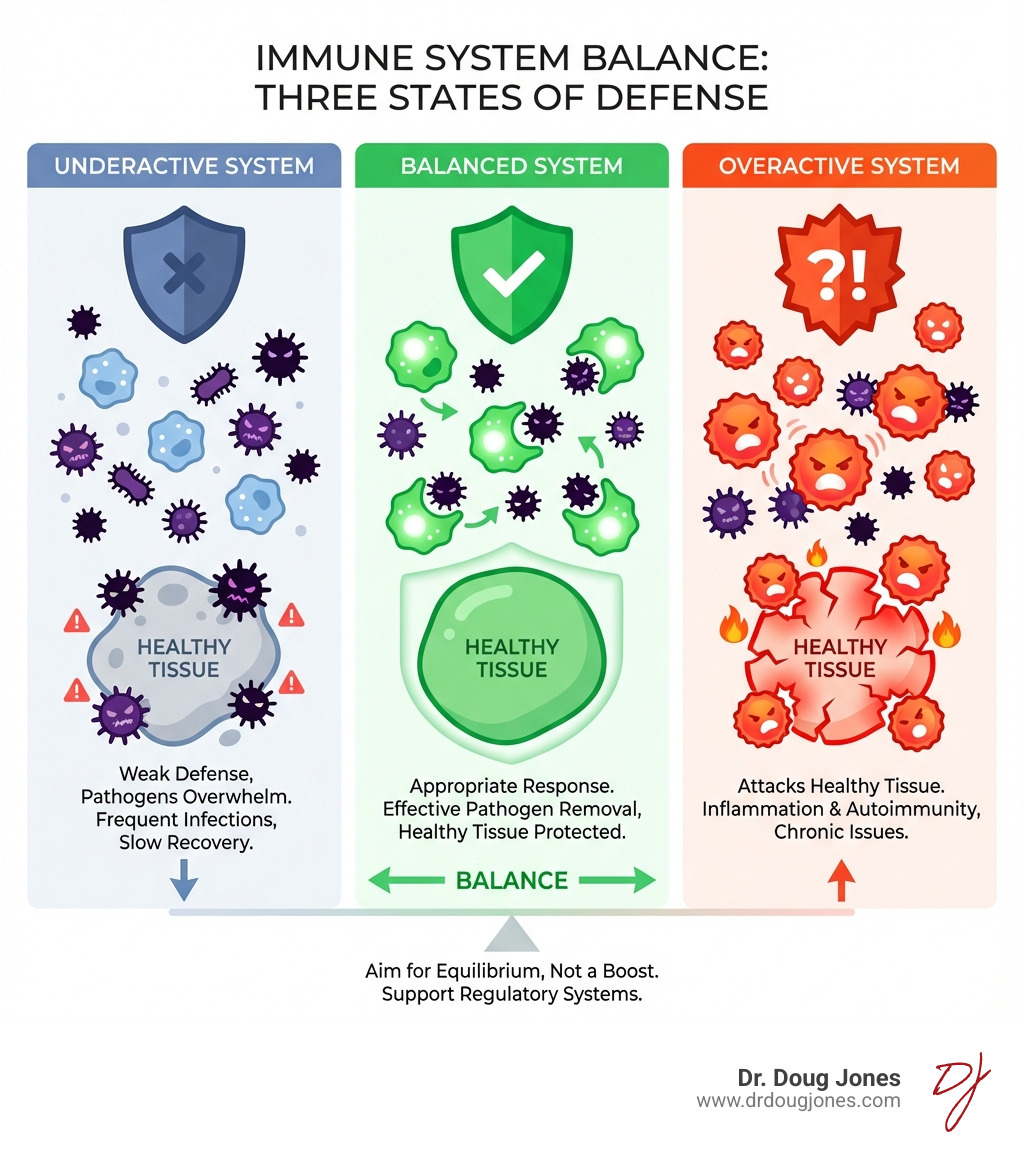
Immune system balance is the key to protecting your body from disease while avoiding harm to your own cells. Unlike popular claims about "boosting" immunity, your immune system functions best when it's in perfect equilibrium—not ramped up or suppressed. "Boosting" your immune system is not a scientific term, rather a marketing term that has no real meaning other than to get you to buy a test or a product. Don't be manipulated by it. We want our immune system optimized by bringing "balance to our immune force."
What Immune System Balance Means:
- Too Strong: Leads to allergies, autoimmune diseases (like lupus or rheumatoid arthritis), and chronic inflammation
- Too Weak: Results in frequent infections, slow healing, and increased cancer risk
- Just Right: Defends against pathogens while sparing healthy tissue through precise regulation
The immune system performs a delicate balancing act every single day. It patrols your body hunting for threats like bacteria, viruses, and cancer cells—while simultaneously checking itself to avoid attacking your own healthy tissues. This isn't about having "more" immunity. Millions of immune cells are actually destroyed daily during training to prevent them from attacking your body.
When this balance tips too far in either direction, disease follows. An overactive immune system mistakes your own cells as enemies, triggering conditions from seasonal allergies to severe autoimmune disorders. An underactive system leaves you vulnerable to infections that your body should easily handle.
The truth: You can't "boost" your way to better immunity. You can only optimize the complex regulatory systems that maintain this critical balance.
As a board-certified immunologist with over a decade treating complex immune conditions including food allergies, autoimmune diseases, and long COVID, I've seen how understanding immune system balance transforms patient outcomes. My work at GAIN—Global Allergy Immune Network—focuses on helping individuals restore this equilibrium and find lasting relief.
The Science of Self-Control: How Your Immune System Maintains Peace
Imagine your immune system as a highly trained security force for your body. Its primary mission is to identify and neutralize threats—anything from a common cold virus to a dangerous bacterium. But here's the tricky part: it must do this without harming the innocent civilians, which are your own healthy cells and tissues. This crucial ability is called immune tolerance, and it's fundamental to maintaining immune system balance.
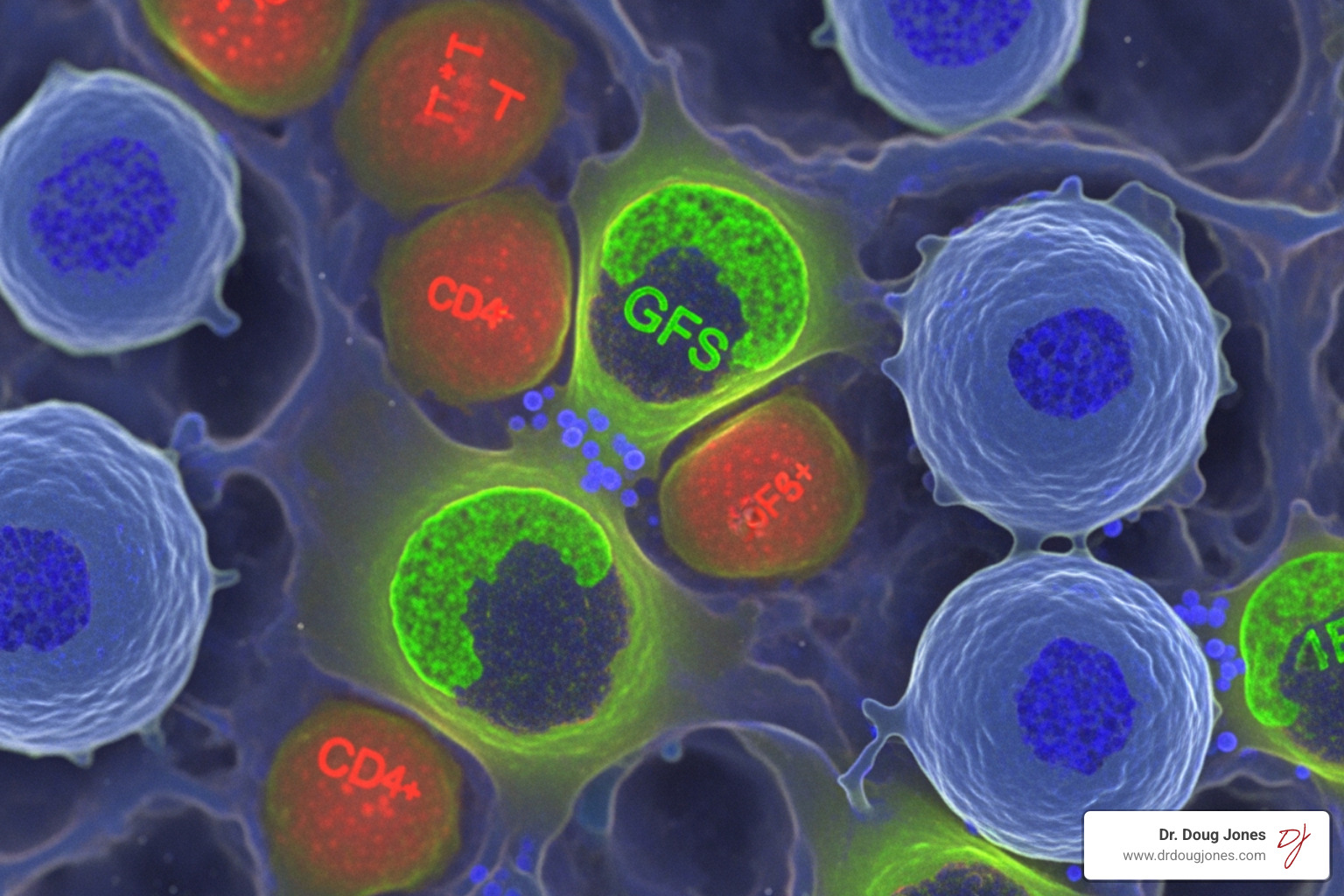
The remarkable feat of distinguishing between "self" (your body's own components) and "non-self" (foreign invaders) is a complex process. It involves specialized immune cells, primarily B cells and T cells, undergoing rigorous training from the moment they are created. These cells are born in places like your bone marrow and thymus, where they learn to recognize friend from foe. For more information about how these amazing cells work, you can explore our guide on More info about the immune system.
During this training, any B cell or T cell that shows signs of "autoreactivity"—meaning it might attack your own body—is typically eliminated. In fact, millions of newly created B and T cells are killed every single day because they fail this critical test. This process, primarily occurring in the central immune organs, is known as central tolerance. It's the first line of defense against self-attack.
However, some self-reactive cells inevitably escape this initial culling and make it into circulation. This is where peripheral tolerance comes into play, acting as a second layer of protection. Here, another crucial set of cells, known as regulatory T cells, or Tregs, patrol the body, ready to suppress any rogue immune responses that could lead to autoimmunity. They're like the internal affairs division, keeping the security force in check.
Groundbreaking Findies in Immune Regulation
The intricate mechanisms of immune tolerance were brought into sharper focus by the groundbreaking research of several key scientists. Their findings revealed how our immune system maintains this delicate equilibrium, revolutionizing our understanding of immune control.
Shimon Sakaguchi's pivotal finding in 1995 identified a new class of immune cells: regulatory T cells (Tregs). He showed that these Tregs act as critical "security guards," actively suppressing immune responses and preventing the immune system from attacking healthy tissues.
Brunkow and Ramsdell then uncovered the molecular key that controls these Tregs. In 2001, they found that mutations in a gene called FOXP3 caused a fatal autoimmune disorder in mice. They later demonstrated that similar mutations in humans lead to a severe autoimmune disease known as IPEX syndrome, characterized by widespread immune dysregulation. Sakaguchi further confirmed in 2003 that the FOXP3 gene is absolutely essential for the development and proper function of regulatory T cells. FOXP3 codes for a transcription factor, a protein that essentially "turns on" the genes needed for Tregs to do their job. Without it, these vital cells either don't form correctly or don't function effectively.
This foundational research highlighted the critical role of Tregs and the FOXP3 gene in preventing autoimmune diseases like Type 1 diabetes, lupus, and rheumatoid arthritis. Their work paved the way for a deeper understanding of immune tolerance and opened new avenues for treating immune-related disorders. If you or someone you know is dealing with these conditions, understanding the immune system's role is key. Learn more about how we can help with Autoimmune Disease Help.
When Tolerance Fails: Consequences of Imbalance
When the immune system's delicate balance is disrupted, and tolerance—the ability to distinguish self from non-self—breaks down, the consequences can be severe. It's like the security force suddenly turning on its own citizens.
One major outcome is autoimmunity. This occurs when the immune system mistakenly identifies the body's own cells and tissues as foreign invaders and launches an attack. Autoimmune diseases such as Type 1 diabetes, lupus, and rheumatoid arthritis are stark reminders of what happens when this self-attack occurs. These conditions can lead to chronic inflammation, tissue damage, and a wide range of debilitating symptoms. The research shows that a breakdown in immune tolerance is a direct cause of autoimmune diseases.
On the other hand, an immune system that is too reactive can lead to allergies and chronic inflammation. In allergies, the immune system overreacts to harmless substances like pollen or certain foods, triggering symptoms ranging from mild discomfort to life-threatening anaphylaxis. We understand that navigating these responses can be challenging; our insights into Food Allergy Immune Response offer more depth. Chronic inflammation, often a silent culprit, can contribute to many modern diseases, including heart disease and certain cancers, even when no active infection is present.
Conversely, if the immune system is underactive or immunodeficient, the body becomes highly vulnerable. Immunodeficiency results when the body doesn't have enough of certain immune cells or if those cells don't function properly. This can be due to genetic factors, certain medications, or conditions like HIV/AIDS. When the immune system is too weak, we face an increased susceptibility to infections, from recurrent colds to severe, life-threatening illnesses. The body struggles to fight off pathogens that a healthy immune system would easily neutralize.
Whether it's an overzealous attack on self or an inability to mount an adequate defense, the message is clear: immune system balance is not just a scientific concept; it's a fundamental requirement for health.
The Myth of 'Boosting' and 'Supporting' vs. the Science of Immune System Balance
You've likely seen countless advertisements and social media posts promising to "boost" or "support" your immune system. While the idea of making your body's defenses stronger sounds appealing, the concept of "immune boosting" is, quite frankly, a scientific inaccuracy that can even be harmful. Those that claim their supplements "support" the immune system are marketing to you. "immune boosters" and "immune support" terms are both manipulative and not scientific. They have no meaning in the science world. Anytime you see or hear those words, that means the product being sold to you has no real scientific data to prove or show anything. If the data existed, they would then make a more specific claim. Since the data does not exist, the companies rely on these terms to market their product.
Our immune system isn't a simple dial you can crank up. Scientific experts, known as immunologists, understand that a healthy immune system doesn't need to be boosted; it functions best when it's perfectly balanced. The goal isn't to have "more" immunity, but to have "just right" immunity.
This myth often leads to a false sense of security, encouraging people to rely on supplements or fad diets rather than truly understanding what their immune system needs. As we've discussed, an immune system that's too active can be just as problematic as one that's underactive, leading to conditions like allergies and autoimmune diseases.
Why More Isn't Better for Your Immune System
Consider this: if you simply "boosted" your immune system by increasing the number of all immune cells, you could quickly run into trouble. Your body already produces vast numbers of immune cells, far more than it needs. Many of these, particularly T cells and B cells (types of lymphocytes), are eliminated through a natural process called apoptosis (programmed cell death) if they are self-reactive or simply surplus to requirements. This constant culling is part of maintaining cellular balance.
If the immune system were a thermostat, turning it up too high would result in overactivation and uncontrolled inflammation. This is precisely what happens in allergies, autoimmune disorders, and chronic inflammatory conditions. Too much of a good thing can indeed be very bad when it comes to our sophisticated internal defense mechanisms. It's why efforts to truly "strengthen" the immune system focus on smart regulation, not brute force. For more insights on this complex topic, refer to our discussion on More on immune strengthening.
The Limitations of "Immunity" Supplements
Given the delicate nature of immune system balance, blindly taking "immunity-boosting" or "immune support" supplements is generally not a good idea. Unless you have a clinically diagnosed micronutrient deficiency, adding more vitamins or herbs won't necessarily make your immune system "better" and could even throw it off balance.
For people with healthy levels of nutrients, taking supplements can lead to a false sense of security. Many dietary supplements carry an important FDA disclaimer stating that their claims have not been evaluated by the FDA and that they are not intended to diagnose, treat, cure, or prevent any disease. This highlights a significant lack of regulation and scientific backing for many products on the market.
We believe that a well-balanced diet, rich in whole foods, is far superior to supplements for providing the necessary micronutrients. Our bodies are designed to absorb nutrients from food efficiently, often alongside other beneficial compounds (like fiber and antioxidants) that supplements can't replicate.
Lifestyle's Role in Supporting a Balanced Immune Response
While we can't "boost" our immune system, we absolutely can—and should—support its ability to maintain immune system balance through healthy lifestyle choices. These aren't quick fixes but rather fundamental pillars of overall health that allow your immune system to function optimally.
A healthy lifestyle encompasses several key areas: a nutritious diet, regular exercise, adequate sleep, and effective stress management. These factors work synergistically, meaning they support each other and contribute to a resilient immune system. As Harvard Health explains, Eating a well-balanced diet, exercising regularly, reducing stress and getting decent sleep can profoundly help your body maintain a functioning and healthy immune system. These behaviors, while not foolproof against every illness, are our best defense.
Nourishing Your Defenses: The Power of Diet and Hydration
What we put into our bodies directly impacts our immune system. A diet rich in a variety of fruits, vegetables, whole grains, and lean proteins provides the essential building blocks and micronutrients our immune cells need.
Key micronutrients vital for immune function include:
- Vitamin B6: Found in fruits (other than citrus) and starchy vegetables like potatoes, as well as poultry, fish, and chickpeas.
- Vitamin C: Abundant in citrus fruits, strawberries, kiwifruit, tomatoes, and red and green bell peppers. While supplements often contain very high doses, your body typically absorbs what it needs from whole foods.
- Vitamin E: Excellent sources include vegetable oils, nuts (like almonds and peanuts), seeds, and green vegetables such as spinach and broccoli.
Beyond nutrients, hydration plays a surprisingly critical role. Water is the main component of lymph, a fluid that carries immune system cells, waste products, and nutrients throughout your body. Staying adequately hydrated ensures that your lymphatic system can efficiently transport these vital components, allowing immune cells to reach where they're needed and waste products to be effectively removed. Practical tips for staying hydrated include carrying a reusable water bottle, setting reminders, and incorporating water-rich foods like melons and cucumbers into your diet. Proper hydration is also a foundational aspect of managing complex immune responses, including those related to Allergy Root Cause.
The Impact of Movement, Rest, and Stress on Immune System Balance
Beyond diet and hydration, other lifestyle factors are equally important for maintaining immune system balance:
- Moderate Exercise: Regular, moderate physical activity contributes to general good health, which in turn supports a healthy immune system. It can help improve circulation, allowing immune cells to move through the body more efficiently. However, extreme or prolonged intense exercise without adequate recovery can temporarily suppress immune function, so balance is key here too!
- Adequate Sleep: Sleep is not just rest; it's a critical period for immune system repair and rejuvenation. During sleep, your body produces and releases cytokines, which are proteins that help fight infection and inflammation. Chronic sleep deprivation can suppress immune function, making you more susceptible to illness. Aim for 7-9 hours of quality sleep per night.
- Stress Management: Chronic stress can have a profound negative impact on your immune system. When you're stressed, your body releases hormones like cortisol, which can suppress immune responses over time. Learning effective stress reduction techniques—such as meditation, deep breathing exercises, spending time in nature, or engaging in hobbies—can help keep these stress hormones in check and support your immune system's ability to maintain balance.
By integrating these healthy habits into your daily life, you provide your immune system with the best possible environment to perform its complex, balancing act effectively.
Immune Balance Across the Lifespan and in Modern Medicine
The quest for immune system balance isn't static; it evolves throughout our lives and is at the forefront of modern medical advancements. From the natural changes that come with aging to sophisticated new therapies for cancer and organ transplantation, understanding and manipulating immune equilibrium holds immense promise.
Aging, Vaccines, and Maintaining Immune System Balance
As we age, our immune system naturally undergoes changes, a process known as immunosenescence. Our immune response capability becomes reduced, which unfortunately contributes to an increased susceptibility to infections and even cancer. This is why respiratory infections, including influenza, the COVID-19 virus, and particularly pneumonia, are leading causes of death in people over 65 worldwide.
One of the key changes is a decrease in the number and effectiveness of T cells, partly due to the thymus (where T cells mature) atrophying with age. This decline means older individuals may not mount as strong an immune response to new infections or even to vaccines compared to younger people.
This is precisely where vaccines play a vital role in maintaining immune system balance throughout life. Vaccines work by introducing harmless forms of pathogens to your body, essentially "training" your immune cells to recognize and fight them. This creates immunological memory, so if you encounter the real, harmful pathogen later, your immune system can quickly mount an effective defense. For older adults, even if vaccine effectiveness is slightly reduced, it still significantly lowers rates of sickness and death compared to no vaccination at all. Vaccines are highlighted as the only safe and effective tool, beyond healthy lifestyle behaviors, to support your immune system.
Understanding how vaccines interact with our immune system is crucial for informed health decisions. We've explored the nuances of immune responses in conditions like Understanding Post-Vaccine Syndrome: Giving a Voice to the Unheard.
The Double-Edged Sword: Immunity in Cancer and Transplantation
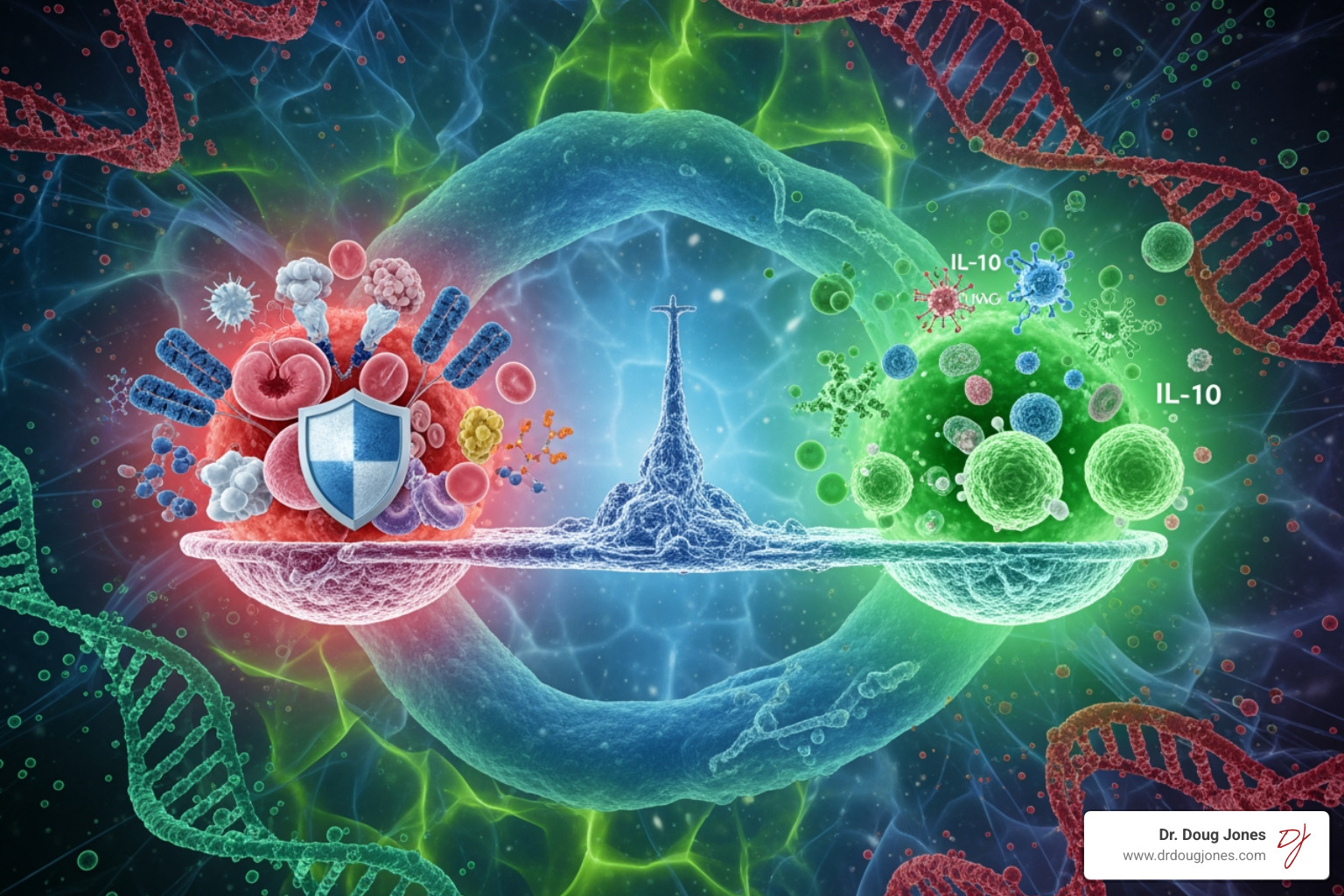
The delicate balance of the immune system can be a double-edged sword in critical medical scenarios like cancer and organ transplantation.
In cancer, regulatory T cells (Tregs), which normally prevent autoimmunity, can sometimes become "too effective" in suppressing immune responses within the tumor's microenvironment. This allows cancer cells to evade detection and destruction by the immune system, leading to tumor growth. However, the understanding of Tregs and the FOXP3 gene has launched a new era in immunotherapies. For cancer, researchers are exploring ways to inhibit Tregs, effectively taking the "brakes" off the immune system so it can more aggressively target and eliminate tumor cells. This is exemplified by the development of immune checkpoint inhibitors, such as those targeting CTLA-4. CTLA-4 is a key negative regulator of T cell function, and its blockade can reverse immunosuppression in the tumor microenvironment, leading to the regression of established cancers. You can read more about this cutting-edge research on immune checkpoints in cancer.
Conversely, in organ transplantation, the challenge is the opposite: we want to promote immune tolerance. The immune system naturally recognizes a transplanted organ as "non-self" and mounts an attack, leading to rejection. Here, researchers are exploring ways to boost the function of Tregs, or even engineer and expand them, to help the body accept transplanted tissues over the long term. This would be a monumental step in improving transplant success rates and reducing the need for lifelong immunosuppressive drugs.
These areas of research underscore how deeply our understanding of immune system balance informs future medical treatments and therapies, from fighting diseases like cancer to ensuring the success of life-saving transplants. The intricate interplay of immune cells and their regulatory mechanisms also provides insights into conditions like Long COVID Symptoms, where immune dysregulation is a significant factor.
Frequently Asked Questions about Immune Balance
What's the difference between "boosting" and "balancing" the immune system?
Boosting is a marketing term implying you can ramp up your immune system, which is scientifically inaccurate and can lead to overactivity like inflammation or autoimmunity. Balancing refers to supporting the immune system's natural state of equilibrium, ensuring it responds appropriately to threats without attacking the body itself. We don't want an immune system that's always "on"—we want one that's smart, responsive, and knows when to stand down.
Can I get all the necessary immune-supporting nutrients from my diet?
For most healthy individuals, a well-balanced diet rich in fruits, vegetables, lean proteins, and whole grains provides all the necessary micronutrients for proper immune function. Our bodies are incredibly efficient at extracting these nutrients from whole foods. Supplements are typically only needed in cases of a diagnosed clinical deficiency, confirmed by a healthcare professional.
How do I know if my immune system is out of balance?
Signs of an underactive immune system often include frequent infections (like recurrent colds, flu, or pneumonia), slow wound healing, and persistent fatigue. Signs of an overactive immune system can manifest as allergies (seasonal, food, environmental), asthma, and symptoms of autoimmune conditions like chronic joint pain, skin rashes (e.g., lupus), digestive issues (e.g., celiac disease), or persistent fatigue. If you suspect your immune system is out of balance, consulting a healthcare professional is crucial for proper diagnosis and guidance.
Conclusion: Your Path to Lasting Immune Harmony
Our journey through the intricate world of the immune system reveals a profound truth: the path to optimal health lies not in "boosting" but in achieving immune system balance. Like a finely tuned orchestra, every component of your immune system must work in harmony, knowing when to act decisively and when to temper its response.
We've seen that an overactive immune system can lead to debilitating autoimmune diseases and allergies, while an underactive one leaves us vulnerable to infections. The groundbreaking findings of regulatory T cells and the FOXP3 gene underscore the scientific community's deep commitment to understanding these delicate mechanisms.
The good news is that we have significant power to support this balance through everyday choices. A healthy lifestyle—encompassing a nutrient-rich diet, adequate hydration, regular moderate exercise, sufficient sleep, and effective stress management—provides the essential foundation for a resilient and well-regulated immune system. As we steer life, our understanding of immune system balance will continue to inform our choices, from embracing the protective power of vaccines to envisioning future therapies for cancer and organ transplantation.
As a board-certified immunologist, I emphasize that understanding these core principles is not just academic; it's empowering. It's about making informed choices that lead to long-term health and lasting relief from complex immune challenges. We encourage you to continue learning and partnering with healthcare professionals to achieve your optimal immune system balance.

