Beyond the Symptoms: Discovering Your Allergy's True Origin
Discover your allergy root cause. Uncover the genetic & environmental factors, diagnosis, and modern strategies for lasting relief.
Why Understanding Your Allergy Root Cause Changes Everything
The allergy root cause isn't just about what triggers your symptoms - it's about understanding why your immune system mistakes harmless substances for dangerous invaders in the first place.
Quick Answer: What Causes Allergies?
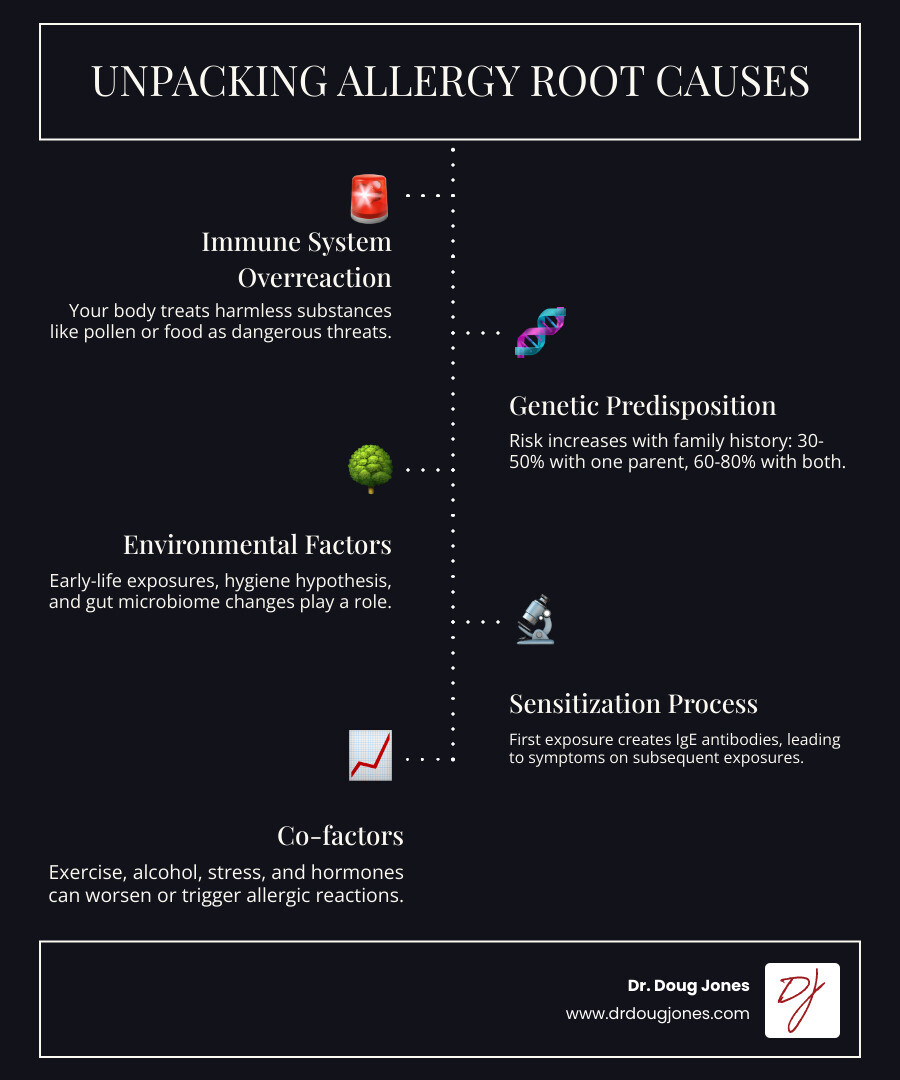
- Immune System Overreaction: Your body treats harmless substances (allergens) as threats
- Genetic Predisposition: 30-50% risk if one parent has allergies, 60-80% if both do
- Environmental Factors: Early-life exposures, hygiene hypothesis, gut microbiome changes
- Sensitization Process: First exposure creates IgE antibodies, second exposure triggers symptoms
- Co-factors: Exercise, alcohol, stress, and hormones can worsen reactions
For up to 50 million American adults, the immune system mistakes harmless substances like pollen or pet dander for dangerous invaders. This happens through a process called sensitization, where the body creates specific IgE antibodies. These antibodies attach to certain cells, waiting for the next encounter. When re-exposure occurs, they trigger the release of histamine and other chemicals, causing symptoms from a runny nose to life-threatening anaphylaxis.
But the real story isn't just what you're allergic to—it's why your immune system learned to react this way. The answer involves a fascinating interplay between your genes and your early-life environment. Research shows that having one allergic parent gives you a 30-50% chance of developing allergies, while two allergic parents bumps that risk to 60-80%.
I'm Dr. Doug Jones, a board-certified immunologist who has spent over a decade helping patients with complex immune conditions understand their allergy root cause and find lasting relief. Through my work at GAIN (Global Allergy Immune Network), I've seen how addressing the underlying immune dysfunction - not just managing symptoms - can transform lives.
The Allergic Cascade: How a Harmless Substance Becomes a Threat
Think of your immune system as an overzealous security guard. It encounters something innocent, like pollen or a food protein, and mistakenly flags it as a threat. This allergy root cause—the immune system's mistaken identity crisis—sets off a chain reaction.
![IMAGE illustrating the sensitization and reaction process with IgE antibodies and mast cells]
The process unfolds in two acts. First is sensitization. On your first encounter with an allergen, your immune system takes notes. B cells and T cells work together to produce specific antibodies called Immunoglobulin E (IgE). Each IgE antibody is designed to recognize only one specific allergen. These IgE antibodies then attach to mast cells and basophils, which are stationed in your skin, lungs, nose, gut, and bloodstream. Once these cells are armed with IgE, you are "sensitized."
The real fireworks happen on the second exposure. The allergen is immediately recognized by the IgE antibodies, triggering the mast cells and basophils to release their chemical arsenal, most notably histamine.
Histamine acts like a fire alarm. It causes blood vessels to leak (leading to swelling), makes nerves itch, and ramps up mucus production. This cascade of chemical mediators creates the classic allergy symptoms: a runny nose, relentless itching, sneezing, and inflammation. It's your immune system's version of using a sledgehammer to swat a fly.
Why Are Allergies So Selective?
Ever wonder why you react to oak trees but not maples? The answer is allergen specificity. Your IgE antibodies recognize exact protein structures. If two substances have different protein fingerprints, your body treats them separately.
Sometimes, however, your immune system gets confused by look-alikes. This is called cross-reactivity. It happens when proteins in different substances are so similar that your IgE antibodies can't tell them apart. A common example is Food Pollen Syndrome or Oral Allergy Syndrome: if you're allergic to birch pollen, you might react to raw apples because their proteins look similar to your immune system. Similarly, a ragweed allergy can cause reactions to melons.
Understanding this mistaken identity is key to finding treatments that go beyond just managing symptoms.
Unpacking the Allergy Root Cause: Genes, Environment, and the Hygiene Hypothesis
Why do some people develop allergies while others don't? The allergy root cause isn't one thing but a perfect storm of factors. Your genetic makeup sets the stage, but your environment—especially during your early years—determines whether that potential becomes reality. Genetics loads the gun, but environment pulls the trigger.
The Genetic Component: Is the Allergy Root Cause in Your DNA?
Family history plays a huge role in allergy development. You don't inherit a specific allergy, but rather a general tendency for your immune system to overreact—an "atopic" tendency.
Here's what the numbers tell us: if one parent has allergies, you have a 30-50% chance of developing them. If both parents are allergic, that jumps to 60-80%. Scientific research on genetic factors in allergy continues to identify specific genes involved, and some studies suggest there might be sex-linked patterns in how allergies are passed down.
Exploring the Environmental Allergy Root Cause: Early Life and Beyond
Genetics may load the gun, but your environment often pulls the trigger. The Hygiene Hypothesis is a key concept here. It suggests that our modern, ultra-clean environments deprive our immune systems of the early exposure to germs needed to properly distinguish friend from foe. Without this training, the immune system may overreact to harmless substances. For example, children who grow up on farms have significantly lower allergy rates.
Your gut microbiome—the community of bacteria in your intestines—is a major player. Factors like C-section versus vaginal birth and early antibiotic use can alter the gut bacteria that help train your immune system. Further, early use of antacids can alter the pH in the stomach which impacts the digestion of foods so the intestines "see" different food proteins.
The timing of allergen exposure is also critical. The dual-allergen exposure hypothesis suggests that eating potential allergens early in life promotes tolerance. In contrast, exposure through damaged skin (like in babies with eczema) can lead to sensitization. This is why early oral introduction of allergenic foods is now recommended.
This learning process isn't limited to childhood. Adult-onset allergies are common, with nearly half of adult food allergies appearing later in life. Moving to a new area, getting a pet, or hormonal changes can all trigger new sensitivities, proving your immune system is constantly adapting.
Identifying Your Triggers: Diagnosis, Co-factors, and Related Conditions
Once you understand the root cause of allergies, the next step is identifying your specific triggers. This detective work helps distinguish a true allergy from other sensitivities.
| Feature | True Allergy | Non-Allergic Intolerance |
|---|---|---|
| Immune System | Involves IgE antibodies and immune response | No immune system involvement |
| Mechanism | Body mistakes harmless substance for threat | Body lacks enzymes or has chemical sensitivity |
| Symptoms | Hives, swelling, breathing problems, anaphylaxis | Digestive issues, headaches, fatigue |
| Severity | Can be life-threatening | Uncomfortable but not dangerous |
| Amount Needed | Tiny traces can trigger severe reactions | Usually needs larger amounts |
| Timing | Rapid onset (minutes to 2 hours) | Can be immediate or delayed (hours to days) |
How Allergies Are Diagnosed
Diagnosing allergies begins with your story—a detailed medical history and physical exam to identify patterns. Based on this, we may use several tests:
- Skin Prick Test: The most common method. A tiny amount of allergen is placed on the skin. A reaction (a small bump) within 20 minutes indicates a possible allergy.
- Specific IgE Blood Test: Measures the amount of IgE antibodies to specific allergens in your blood. It's useful when skin tests aren't an option.
- Patch Test: Used for contact allergies (like nickel or latex). Patches with allergens are worn on the skin for 48-72 hours to check for a delayed reaction.
- Oral Food Challenge: The gold standard for food allergies. Under strict medical supervision, you consume gradually increasing amounts of a food to confirm or rule out an allergy.
- Elimination Diets: Involves temporarily removing suspected foods and then reintroducing them to track symptoms.
Crucially, interpreting test results requires expertise. A positive test doesn't always mean a clinical allergy. We combine test results with your clinical history for an accurate diagnosis.
Common Allergens and Co-factors That Worsen Reactions
Allergens are everywhere. Key categories include:
- Airborne Allergens: Pollen (from trees, grasses, weeds), dust mites, mold spores, and pet dander.
- Food Allergens: The "Big 9" (milk, eggs, peanuts, tree nuts, soy, wheat, fish, shellfish, and sesame) account for 90% of serious reactions.
- Other Allergens: Insect stings (bees, wasps), drug allergies (penicillin), and contact allergens (nickel, latex).
It's not just the allergen that matters. Co-factors can lower your reaction threshold, turning a mild sensitivity into a major problem. These include:
- Exercise, especially when combined with certain foods.
- Alcohol and NSAIDs (like ibuprofen).
- Stress, infections, and hormonal changes (menstrual cycle, pregnancy, menopause).
Allergic diseases are often linked. The "atopic march" describes the common progression from infant eczema to food allergies, allergic rhinitis, and asthma. Understanding these connections is key to comprehensive care.
From Management to Modification: Modern Strategies for Lasting Relief
While avoiding triggers and managing symptoms is important, our understanding of the allergy root cause has led to treatments that can change how your immune system responds. Instead of just putting a band-aid on the problem, we can now address the underlying immune dysfunction.

Symptom Control vs. Disease-Modifying Treatments
Think of allergy treatment as dealing with a leaky roof. You can place buckets to catch drips (symptom control) or fix the roof itself (disease modification).
Symptom control treatments offer fast relief. Antihistamines block histamine, while nasal corticosteroids reduce inflammation in the nose. Decongestants clear stuffiness but should be used short-term. These manage symptoms but don't change the underlying allergy.
Disease-modifying treatments retrain your immune system. Allergen immunotherapy (allergy shots or under-the-tongue drops) gradually exposes you to your allergen, teaching your body tolerance over time. For severe cases, biologics like anti-IgE therapy can target specific parts of the allergic response. You can learn more about sublingual options through resources at Hopkins Medicine. These treatments address the allergy root cause for lasting change.
The Power of Prevention: Early Introduction and Avoidance
For decades, the advice was to avoid giving allergenic foods to babies. Groundbreaking research, like the LEAP study, completely reversed this thinking.
The study found that high-risk infants who were regularly fed peanut products from an early age had an 80% reduction in peanut allergy risk. This protection was long-lasting. You can read the detailed evidence from the LEAP study that reshaped prevention strategies.
Following this, the American Academy of Pediatrics now recommends early introduction of allergenic foods for most infants. It turns out that for prevention, early exposure is often better than avoidance.
Of course, once an allergy is established, strict avoidance is critical. While some childhood allergies (milk, egg) are often outgrown, others (peanut, tree nut) tend to be lifelong. Never assume an allergy is gone without medical testing.
Preparing for the Worst: Anaphylaxis Prevention and Response
While most reactions are mild, some people can experience anaphylaxis, a severe, life-threatening reaction. You are at higher risk if you have a history of severe reactions, asthma, or certain food, insect, or drug allergies.
Preparation is key. If you are at risk, you must carry two epinephrine auto-injectors at all times. A second dose may be needed before help arrives.
Work with your doctor to create a clear emergency action plan. This plan should list your allergens, describe your specific symptoms, and state when and how to use epinephrine. Wearing a medical alert bracelet and ensuring family, friends, and colleagues know how to help is also vital.
If you suspect anaphylaxis, use epinephrine immediately and call 911. Do not wait for symptoms to worsen—early treatment saves lives.
Frequently Asked Questions about Allergy Causes
After diving deep into the science behind the allergy root cause, you might still have some questions. Here are the most common ones I hear in my practice.
Why did I suddenly develop allergies as an adult?
This is surprisingly common. Nearly half of adult food allergies appear in adulthood. The reasons vary, but common triggers include:
- New Exposures: Moving to a new region with different pollens, getting a new pet, or changing your diet can introduce new allergens to your immune system.
- Immune System Changes: Hormonal shifts (pregnancy, menopause), high stress, or even some medications can alter how your immune system functions.
- Co-factors: Factors like exercise, alcohol, or NSAID use can lower your reaction threshold, unmasking a previously unnoticed sensitivity.
Can you have an allergy if blood or skin tests are negative?
Yes, absolutely. Standard tests primarily detect IgE-mediated allergies, but other immune pathways can cause reactions. For example, some food allergies (like FPIES) and conditions like local allergic rhinitis (where symptoms are confined to the nose) won't show up on these tests. What feels like an allergy could also be a non-immune intolerance or a side effect of medication. This is why a detailed clinical history is just as important as any test result. We must look at the complete picture to understand the true cause of your symptoms.
What is the difference between an allergy and an intolerance?
This is a critical distinction for your safety.
A true allergy is an immune system reaction. Your body mistakes a harmless substance for a threat, creating IgE antibodies and launching an attack. Even a tiny amount can cause symptoms like hives, swelling, breathing trouble, or life-threatening anaphylaxis.
An intolerance does not involve the immune system. It's typically a digestive issue, like the inability to break down a certain food (e.g., lactose intolerance). Symptoms are usually digestive (gas, bloating, diarrhea) and, while uncomfortable, are not life-threatening. The severity often depends on the amount consumed.
Take Control of Your Immune Health
Understanding your allergy root cause is the first step toward changing your health - and it changes everything. When you know why your immune system learned to see harmless substances as threats, you can finally move beyond just managing symptoms to addressing the deeper patterns that drive your reactions.
This isn't about quick fixes or one-size-fits-all solutions. Your immune system is as unique as your fingerprint, shaped by your genetic predisposition, your early-life environmental factors, and the complex dance between your gut microbiome and immune development. Maybe you inherited that 60-80% risk from both allergic parents, or perhaps the hygiene hypothesis explains why your pristine childhood environment left your immune system undertrained.
The good news? Your immune system isn't static. It's constantly adapting and learning, which means there's real potential for immune system regulation and lasting change. Whether your triggers stem from a disrupted gut microbiome, mistimed early exposures, or co-factors like stress and hormones, understanding these root causes opens the door to personalized solutions.
As a board-certified immunologist, I've spent over a decade helping patients solve these complex genetic and environmental factors. Through my work, I've seen how addressing the underlying immune dysfunction - rather than just suppressing symptoms - can lead to genuine, lasting relief. It's about redefining what's possible when you understand your body's unique story.
Your journey starts with recognizing that allergies aren't just something you have to live with. They're a window into your immune system's history and a roadmap to your healing. When we work together to understand your specific allergy root cause, we can develop targeted strategies that honor your body's complexity while empowering you with the knowledge and tools you need.
Ready to find what's really driving your immune challenges and explore solutions designed specifically for you?

