Beyond the Diagnosis: Finding Real Help for Autoimmune Conditions
Seeking Autoimmune disease help? Learn causes, get diagnosed, & implement integrative strategies for relief & lasting health.
Why Understanding Autoimmune Disease is the First Step to Real Relief
Autoimmune disease help starts with understanding why your immune system turns against you. If you have unexplained fatigue, joint pain, digestive issues, or other chronic symptoms, you're not alone—and there is hope.
Quick answers for autoimmune disease help:
- What it is: Your immune system mistakenly attacks healthy tissue.
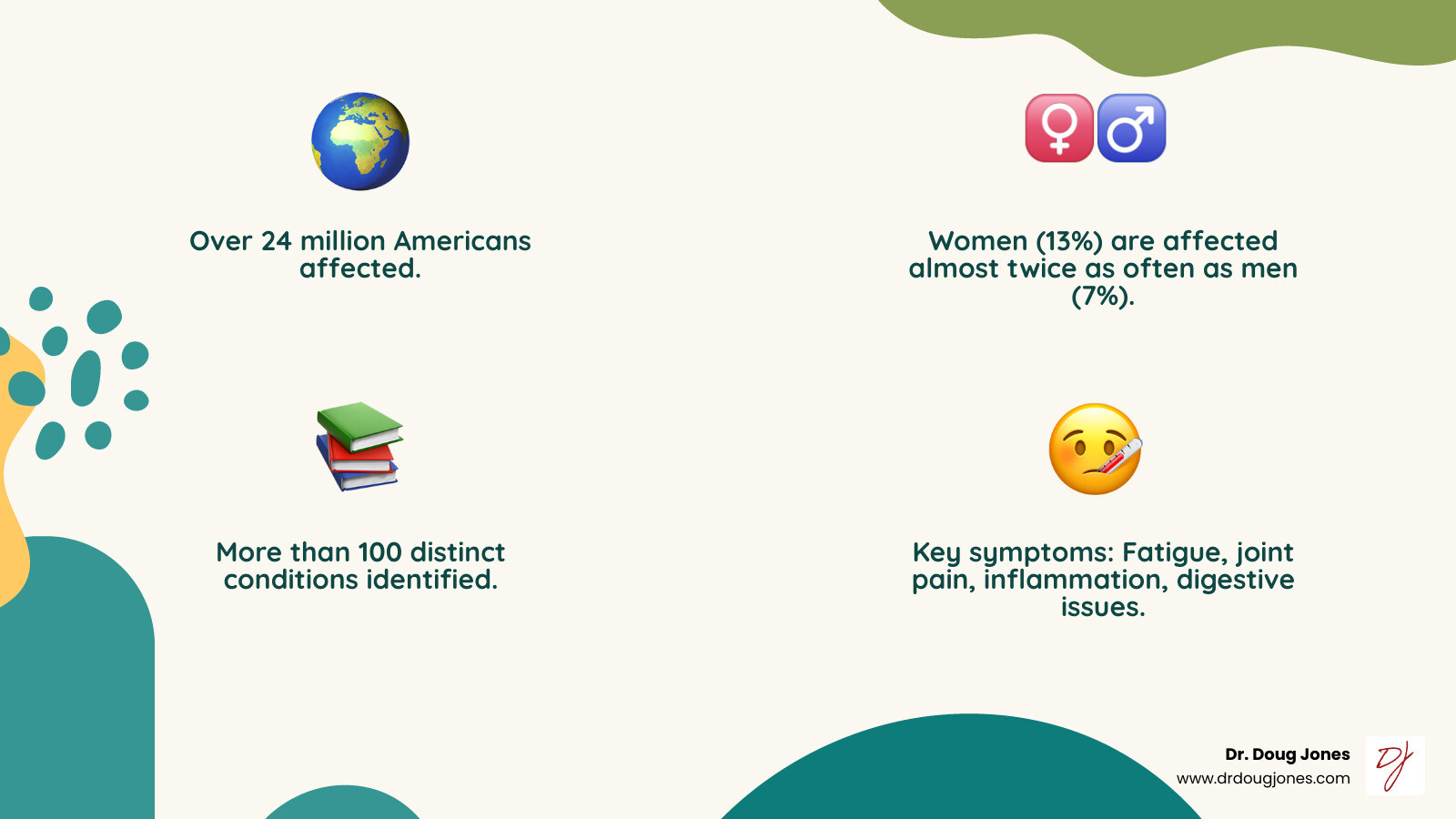
- Who's affected: Over 24 million Americans; women are at higher risk.
- Common signs: Chronic fatigue, joint pain, inflammation, digestive problems, skin issues.
- Hope exists: While there's no cure, remission is possible.
- Next steps: Work with specialists, address root causes, and create a personalized plan.
Autoimmune diseases affect more than 24 million Americans, with over 100 different conditions identified. Women are nearly twice as likely as men to develop them. Behind each diagnosis is a person seeking answers, relief, and hope.
Living with an autoimmune disease can feel confusing and isolating, a feeling often compounded by the long road to a proper diagnosis.
Your immune system is your body's defense force. In autoimmune disease, it gets confused and attacks your own healthy cells. This journey can be overwhelming, with many people spending years seeking answers or being told their symptoms are "all in their head."
I'm Dr. Doug Jones, a board-certified immunologist specializing in complex immune conditions. For over a decade, I've helped thousands of patients find lasting relief. My integrative approach combines conventional medicine with evidence-based natural therapies to address root causes and restore immune balance.
Understanding Autoimmune Disease: When the Body Attacks Itself
Picture your immune system as your body's personal security team. Normally, it distinguishes between you (your cells) and threats (like bacteria and viruses). In autoimmune disease, this system gets confused and starts treating your own healthy cells like dangerous intruders.
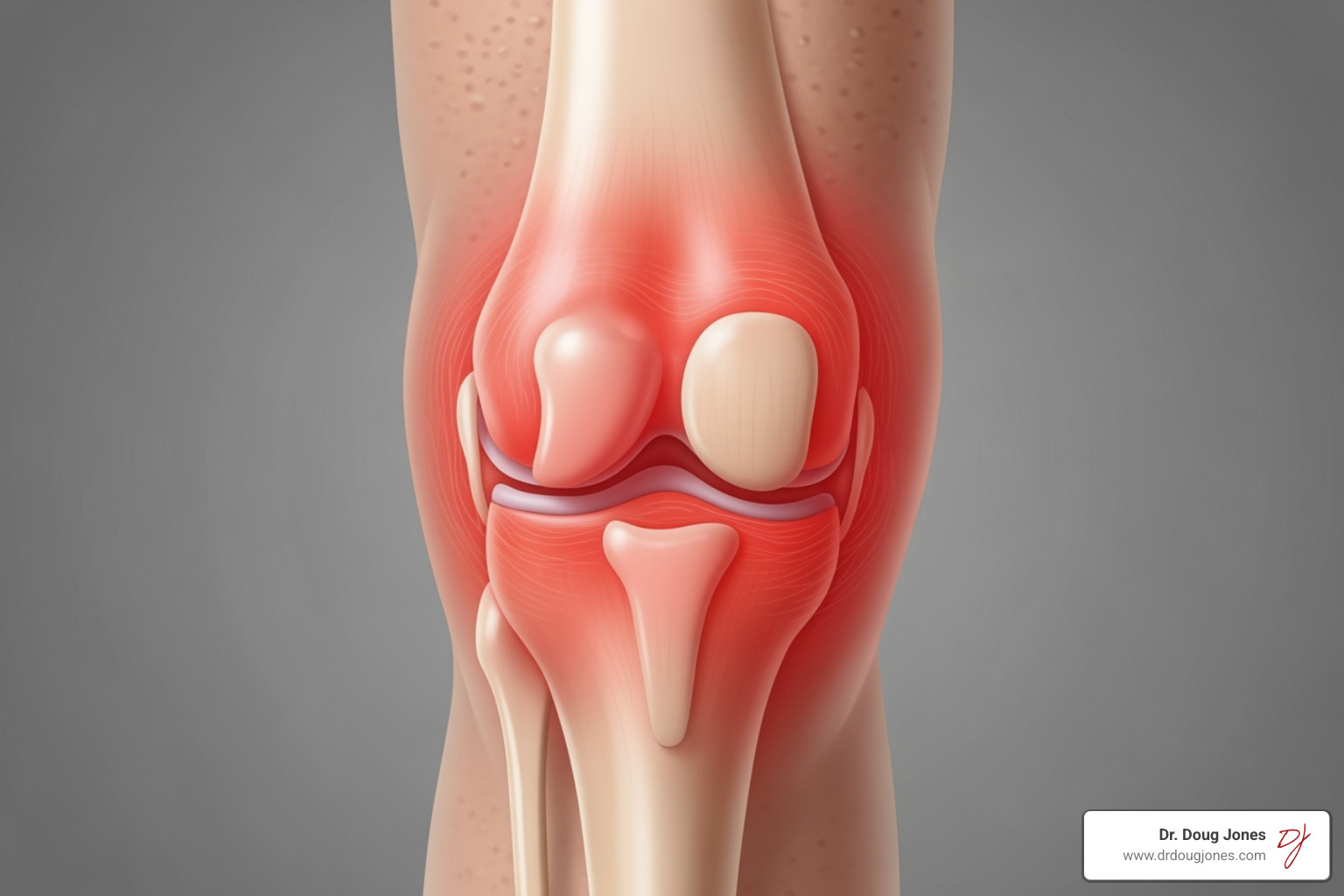
When this happens, your immune system creates autoantibodies that target your own tissues, leading to inflammation—the warmth, redness, swelling, and pain many people with autoimmune conditions experience.
Autoimmune diseases can attack almost any part of your body, including your joints, skin, digestive system, or brain. Where the attack happens determines the type of autoimmune disease and your symptoms.
Most autoimmune diseases follow a frustrating pattern of flares (when symptoms worsen) and remission (when symptoms calm down or disappear). This unpredictability is one of the hardest parts of living with these conditions. Some diseases affect specific organs (like Hashimoto's thyroiditis), while others are systemic and impact multiple parts of your body (like lupus).
While these are chronic conditions, many people find effective ways to reduce symptoms and improve their quality of life. The key is understanding what's happening and working with the right team to address both symptoms and root causes.
For more detailed information, you can consult resources from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the Department of Health and Human Services, and the National Institutes of Health.
Common Symptoms and Conditions
While symptoms vary, some common threads can be the first step toward getting the autoimmune disease help you need.
- Fatigue: A bone-deep exhaustion that doesn't improve with rest.
- Joint pain and swelling: Often symmetrical (affecting both sides of the body), with stiffness that is worse in the morning.
- Skin problems: Rashes, dry patches, hair loss, or changes in skin color.
- Abdominal pain and digestive issues: Bloating, cramping, diarrhea, or constipation, which makes sense as much of your immune system is in your gut.
- Recurring low-grade fevers: Your body runs slightly hot without any obvious infection.
- Swollen glands: Lymph nodes in your neck, armpits, or groin may be swollen.
- Malaise: A general feeling of being unwell without a clear cause.
With over 100 different autoimmune diseases, specific conditions vary widely. Here are a few common examples:
- Rheumatoid arthritis: Primarily targets joints.
- Lupus: Can attack almost any organ system.
- Celiac disease: An immune reaction to gluten that damages the small intestine. People with celiac disease are at higher risk for other Associated Autoimmune Diseases.
- Hashimoto's thyroiditis: Slows down the thyroid.
- Graves' disease: Speeds up the thyroid.
- Type 1 diabetes: Destroys insulin-producing cells.
- Psoriasis: Causes thick, scaly skin patches.
- Multiple sclerosis: Attacks the protective coating around nerves.
- Crohn's disease and ulcerative colitis: Cause chronic gut inflammation.
- Myasthenia gravis: Causes muscle weakness.
It's important to know that having one autoimmune disease increases your likelihood of developing another. This knowledge helps you and your healthcare team stay vigilant for new symptoms and catch additional conditions early.
The Root Causes: Solving the Triggers of Autoimmunity
Understanding what triggers an autoimmune response is key to getting autoimmune disease help. It's rarely just one thing; autoimmunity is more like a perfect storm of genetic and environmental factors.
I often tell my patients that genetics load the gun, but environment pulls the trigger. Even if autoimmune disease runs in your family, you aren't destined to develop one. However, it does mean we need to pay close attention to the factors that can activate those genetic predispositions.
Common environmental triggers include:
- Infections: Some viruses or bacteria look similar to your own cells, a process called "molecular mimicry," causing your immune system to attack both.
- Toxins: Chemicals like BPA from plastics and heavy metals can stimulate immune cells, disrupt hormones, and fuel inflammation.
- Intestinal permeability (leaky gut): When the gut lining is damaged, undigested food particles and toxins can slip into the bloodstream, triggering an immune attack and chronic inflammation.
- Hormonal influence: Hormonal fluctuations, particularly in women, can activate immune responses, which helps explain why women are more affected.
At the heart of all autoimmune conditions is the role of inflammation. Uncontrolled inflammation is the common thread that keeps these diseases active.
The Interplay of Genetics and Environment
A family history is a risk factor, but it doesn't seal your fate. By addressing environmental triggers early, many people can prevent or delay symptoms.
Certain gene mutations (like MTHFR) can make you more susceptible by affecting how your body processes nutrients and toxins. These genes can remain dormant until environmental triggers activate them.
The concept of evolutionary mismatch helps explain the rise in autoimmune diseases. Our bodies evolved for a very different environment. The modern Western diet, full of processed foods, sugar, and inflammatory oils, is mismatched with what our immune systems are designed to handle.
When you combine this diet with chronic stress, poor sleep, and chemical exposures, you create the perfect conditions for immune system confusion. The good news is that understanding these root causes provides a roadmap for healing. By addressing environmental triggers, we can help your body find balance again.
The Path to Diagnosis: Getting Clear Answers
If you've been searching for autoimmune disease help, you've likely experienced the frustrating path to a proper diagnosis. Getting clear answers is challenging because autoimmune diseases are masters of disguise, with symptoms that overlap with many other conditions.
As the National Institute of Arthritis and Musculoskeletal and Skin Diseases notes, diagnosis is difficult due to these overlapping symptoms. Your doctor must act as a detective, ruling out other possibilities in a "differential diagnosis" process.
This is where you become your own best advocate. I encourage patients to keep a detailed symptom journal—noting what you feel, when, and what makes it better or worse. This provides crucial clues that can speed up your diagnosis. As patient advocacy organizations advise, "choosing the right type of doctor early can accelerate diagnosis and care."

Key Diagnostic Tests and Procedures
Your provider will start with a physical exam and a detailed health history. From there, lab tests can look for signs of immune dysfunction and inflammation.
- Antinuclear Antibody (ANA) test: A general screening tool that checks if your immune system is making antibodies against your own cells. A positive result suggests more investigation is needed.
- C-Reactive Protein (CRP) test: Measures general inflammation in your body. You can learn more about this marker from the National Library of Medicine's information on CRP testing.
- Erythrocyte Sedimentation Rate (ESR): Also called a "sed rate," this test measures how quickly red blood cells settle, which is faster when inflammation is present.
- Specific autoantibody tests: If initial tests are positive, your doctor may order targeted tests for antibodies linked to specific conditions, like anti-CCP for rheumatoid arthritis or anti-TPO for Hashimoto's.
- Immunoglobulin A (IgA) blood testing: This test is valuable as IgA protects mucous membranes in the gut and respiratory system. KidsHealth.org provides helpful information on what IgA testing involves.
- Complete Blood Count (CBC): Checks for anemia or signs of infection.
- Comprehensive Metabolic Panel (CMP): Assesses kidney and liver function.
- Urinalysis: Can detect early signs of kidney involvement.
Depending on your symptoms, you might also need imaging tests like X-rays, MRI, or ultrasounds to check for joint damage or organ inflammation. Each test provides another piece of the puzzle, bringing you closer to a clear diagnosis and an effective treatment plan.
A Comprehensive Approach to Autoimmune Disease Help: Integrative Strategies
Effective autoimmune disease help requires looking beyond symptom management. While conventional medicine is excellent for controlling flares, true healing comes from understanding why your immune system is confused. This is the difference between simply managing symptoms and addressing the root cause.
Every person's autoimmune journey is unique, shaped by genetics, environmental exposures, stress, and gut health. This is why a one-size-fits-all approach rarely works. Our personalized care model focuses on managing your current symptoms while investigating the underlying triggers. We also believe in patient empowerment; as advocates say, "immerse yourself in reliable information from trusted sources." Finally, we create a completely custom plan based on comprehensive testing and your unique health story.
Medical Treatments and Supportive Therapies
Conventional medical treatments are the backbone of autoimmune care, working primarily by calming an overactive immune system.
- Immunomodulatory therapies: These are often a first-line defense, ranging from broad immunosuppressants to newer biologics that target specific inflammatory pathways.
- Corticosteroids: Drugs like prednisone offer fast, powerful relief from severe inflammation but are typically used short-term due to side effects.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen and similar drugs can provide relief from pain and inflammation, especially for joint symptoms.
- Specific medications: Some conditions require specific treatments, like insulin for Type 1 diabetes or a strict gluten-free diet for celiac disease.
- Physical therapy: Crucial for maintaining mobility and strength.
- IVIG infusions: These infusions of healthy antibodies can help regulate your immune system.
The National Library of Medicine offers more detail on Autoimmune Disorders and their treatments.
Lifestyle Changes for Autoimmune Disease Help
While medications manage symptoms, lifestyle changes can influence the root causes of immune dysfunction. These are powerful tools for improving how you feel.
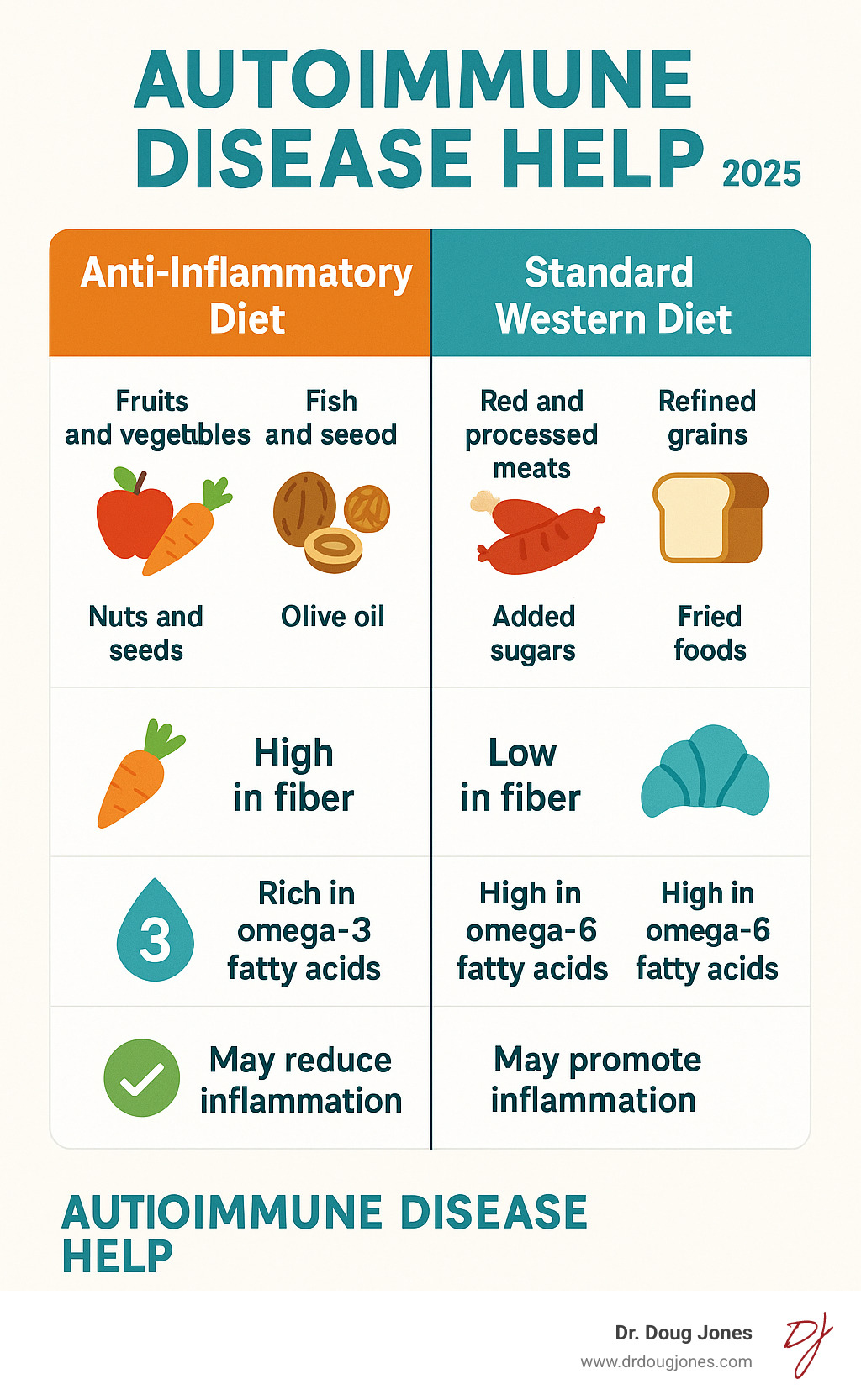
- Anti-inflammatory nutrition: Every meal sends a signal to your immune system. Focusing on nutrient-dense whole foods, healthy fats, and colorful vegetables helps reduce systemic inflammation.
- Gut health: Since about 70% of your immune system is in your gut, supporting it with probiotics, prebiotics, and fermented foods is critical for keeping your immune system calm.
- Stress management: Chronic stress fuels autoimmune inflammation. Practices like meditation, deep breathing, or time in nature can change your immune system's behavior.
- Quality sleep: Restorative sleep is non-negotiable. A lack of sleep impairs the regulatory immune cells that keep autoimmune reactions in check. Aim for 7-9 hours nightly.
- Moderate exercise: Regular movement acts as a natural anti-inflammatory, but the key is moderation to support, not stress, your system.
- Addressing nutrient deficiencies: Key nutrients like Vitamin D and omega-3 fatty acids are crucial for immune regulation. Targeted supplementation with fish oil, vitamin C, and herbs like curcumin can offer additional support.
These lifestyle approaches work together, creating a powerful synergistic effect that can lead to big improvements in your daily life.
Building Your Care Team and Navigating Your Journey
Living with an autoimmune condition isn't a journey to take alone. Building a personal health dream team is essential, and you're the team captain, making the final decisions about your care.
This support system should include more than just medical professionals. As patient advocates note, "it's important for our own mental well-being to have contact with others who have shared experiences." Connecting with people who understand your journey provides real strength.
To work effectively with your healthcare team, come to appointments prepared with a symptom journal, a list of all medications and supplements, and recent test results. The Autoimmune Association offers a free toolkit to help you organize your information. You know your body best. If a treatment isn't working, speak up. Your voice is a crucial part of finding effective autoimmune disease help.

Finding the Right Specialists for Autoimmune Disease Help
Different conditions require different specialists, each bringing focused expertise.
- Rheumatologists: Specialize in joint and muscle-related conditions like rheumatoid arthritis and lupus.
- Endocrinologists: Treat hormone-related conditions like Hashimoto's thyroiditis, Graves' disease, and Type 1 diabetes.
- Gastroenterologists: Focus on digestive disorders like Crohn's disease, ulcerative colitis, and celiac disease.
- Neurologists: Provide care for nervous system conditions like multiple sclerosis and myasthenia gravis.
- Dermatologists: Handle skin-related conditions like psoriasis and vitiligo.
- Integrative and functional medicine practitioners: Look beyond symptoms to identify root causes, offering approaches that complement conventional care.
The American College of Rheumatology can help you find specialists. For integrative support, consult directories from The Institute for Functional Medicine or the American Association of Naturopathic Physicians.
The Long-Term Outlook: Can Remission Be Achieved?
The most pressing question is often: Can I actually get better? While there is no traditional "cure" for autoimmune diseases, remission is absolutely possible. Remission means long periods where symptoms are minimal or have disappeared entirely.
Many of our patients achieve remission and dramatically improve their quality of life through a comprehensive approach that addresses both symptoms and root causes.
Our goals are to:
- Reduce flare frequency and severity: By addressing triggers, flares become less common and intense.
- Improve quality of life: Significantly reducing chronic pain, fatigue, and other symptoms can transform your daily experience. Research shows that stress management alone can improve well-being.
- Empower you with control: Understanding your body and its triggers puts you in the driver's seat of your health journey.
Success stories prove that a personalized, root-cause approach can lead to profound healing and renewed vitality.
Conclusion
By seeking autoimmune disease help, you're taking the most important step: becoming informed and empowered about your health. Living with an autoimmune condition doesn't have to mean a life of constant symptoms and uncertainty.
We've explored how these diseases develop, the interplay of genetics and environment, and a path forward that goes beyond just managing symptoms.
The integrative approach focuses on the whole picture. Conventional treatments are crucial for controlling flares, but true healing happens when we also address root causes—supporting gut health, managing stress, optimizing sleep, and embracing anti-inflammatory nutrition.
This isn't about quick fixes. Autoimmune diseases are chronic, but many people do achieve significant remission and dramatically improved quality of life with a comprehensive approach. You are not defined by your diagnosis; you have the power to influence your health outcomes.
The future of autoimmune care is bright, with exciting developments in personalized medicine and a better understanding of the gut-immune connection.
As Dr. Doug Jones, a board-certified immunologist, I've dedicated my career to redefining how we approach complex immune challenges. My experience shows that when we combine cutting-edge science with personalized care, remarkable healing is possible. Your journey is unique, and your care should be too.
Your autoimmune journey doesn't end with a diagnosis—it's a new beginning. With the right knowledge and support, you can take control of your health and work toward the vibrant life you deserve.
Ready to explore what a personalized approach might look like for your specific situation?
