Chronic Stomach Pain and Autoimmune Disorders: A Comprehensive Guide
Navigate auto immune disorder chronic stomach pain. Get a comprehensive guide on causes, diagnosis, & effective treatment.

Understanding the Connection Between Your Immune System and Persistent Stomach Pain
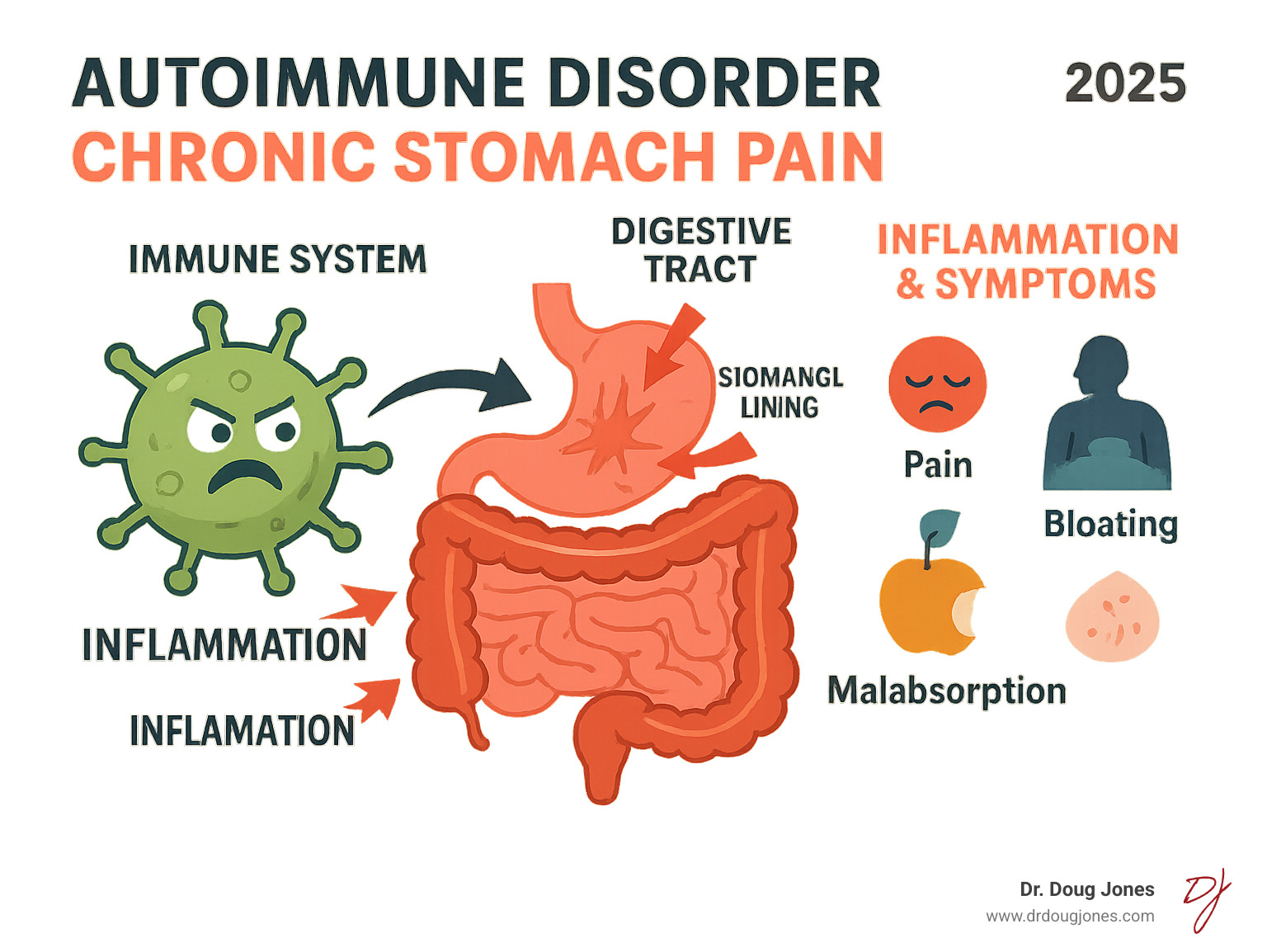
Auto immune disorder chronic stomach pain affects millions of people who struggle with persistent digestive symptoms that seem to have no clear cause. When your immune system mistakenly attacks healthy tissue in your digestive tract, it can create ongoing inflammation and pain that significantly impacts your quality of life.
Common autoimmune disorders that cause chronic stomach pain include:
- Autoimmune gastritis - immune attack on stomach lining cells
- Inflammatory bowel disease (IBD) - includes Crohn's disease and ulcerative colitis
- Celiac disease - autoimmune reaction to gluten
- Systemic lupus - can affect the entire digestive system
- Systemic sclerosis - causes digestive motility problems
The statistics are striking: autoimmune diseases affect 23.5 million Americans, with nearly 80% being women. Many of these conditions can cause chronic abdominal pain, bloating, digestive issues, and nutrient deficiencies that leave patients feeling exhausted and frustrated.
The key difference between autoimmune digestive disorders and other stomach problems is that your body's own defense system becomes the problem. Instead of protecting you, your immune system creates inflammation that damages healthy tissue in your gut.
I'm Dr. Doug Jones, a board-certified immunologist who has spent over a decade helping patients with complex immune conditions, including those experiencing auto immune disorder chronic stomach pain. Through my practice at GAIN (Global Allergy Immune Network), I've seen how proper diagnosis and comprehensive treatment can transform lives for people struggling with these challenging conditions.
The Gut-Immune Connection: Why Your Body Might Attack Itself
Your digestive system is a key player in your body's defense, housing roughly 70% of your entire immune system. This network, known as Gut-Associated Lymphoid Tissue (GALT), acts as a first line of defense, with immune cells that monitor everything passing through. They are highly effective—until something goes wrong.

Autoimmunity occurs when the immune system malfunctions, mistakenly identifying healthy cells as invaders. This self-attack leads to chronic inflammation and the persistent stomach pain many patients experience. This malfunction is rarely caused by a single factor, but rather a combination of triggers.
Genetics can create a predisposition for autoimmunity. If these diseases run in your family, you may be more vulnerable, but genes alone don't guarantee you'll develop auto immune disorder chronic stomach pain. They simply set the stage for other triggers.
Environmental factors can be the tipping point. Certain infections (like H. pylori bacteria), exposure to toxins, chronic stress, or even some medications can flip the switch on autoimmune responses in people who are genetically prone to them.
The gut microbiome, or the balance of bacteria, is also crucial. An imbalance, known as gut dysbiosis, can lead to a more permeable intestinal barrier or "leaky gut." This allows substances to pass into the bloodstream, triggering an immune attack.
Another trigger is molecular mimicry, where proteins from an infection resemble your body's own proteins. The immune system learns to attack the invader and then continues to attack similar-looking native tissues.
When this immune confusion targets your digestive system, the result is often chronic inflammation that can cause persistent stomach pain, digestive upset, and a cascade of other symptoms that can significantly impact your daily life.
Key Autoimmune Disorders Behind Chronic Stomach Pain
When your immune system turns against your digestive tract, the results can be both painful and puzzling. Auto immune disorder chronic stomach pain manifests differently depending on which part of your digestive system becomes the target. Let's explore the most common autoimmune conditions that cause persistent stomach discomfort.
Autoimmune Gastritis (AAG): The Stomach Under Attack
In autoimmune gastritis (AAG), the immune system attacks the stomach's parietal cells, which produce stomach acid and intrinsic factor (essential for vitamin B12 absorption).
This attack leads to low stomach acid (achlorhydria), causing bloating and early satiety (feeling full quickly). The damage to intrinsic factor prevents B12 absorption, leading to pernicious anemia. Symptoms often develop slowly and include upper abdominal pain, a heavy feeling in the stomach, and overwhelming fatigue. As B12 deficiency worsens, neurological symptoms like tingling in the hands and feet or memory issues can appear.
AAG affects an estimated 0.5% to 2% of people in the U.S. and is often associated with other autoimmune conditions like Hashimoto's thyroiditis and Type 1 diabetes. If you have an existing autoimmune disease and new stomach pain, AAG should be considered. More on autoimmune gastritis.
Inflammatory Bowel Disease (IBD): Crohn's & Ulcerative Colitis
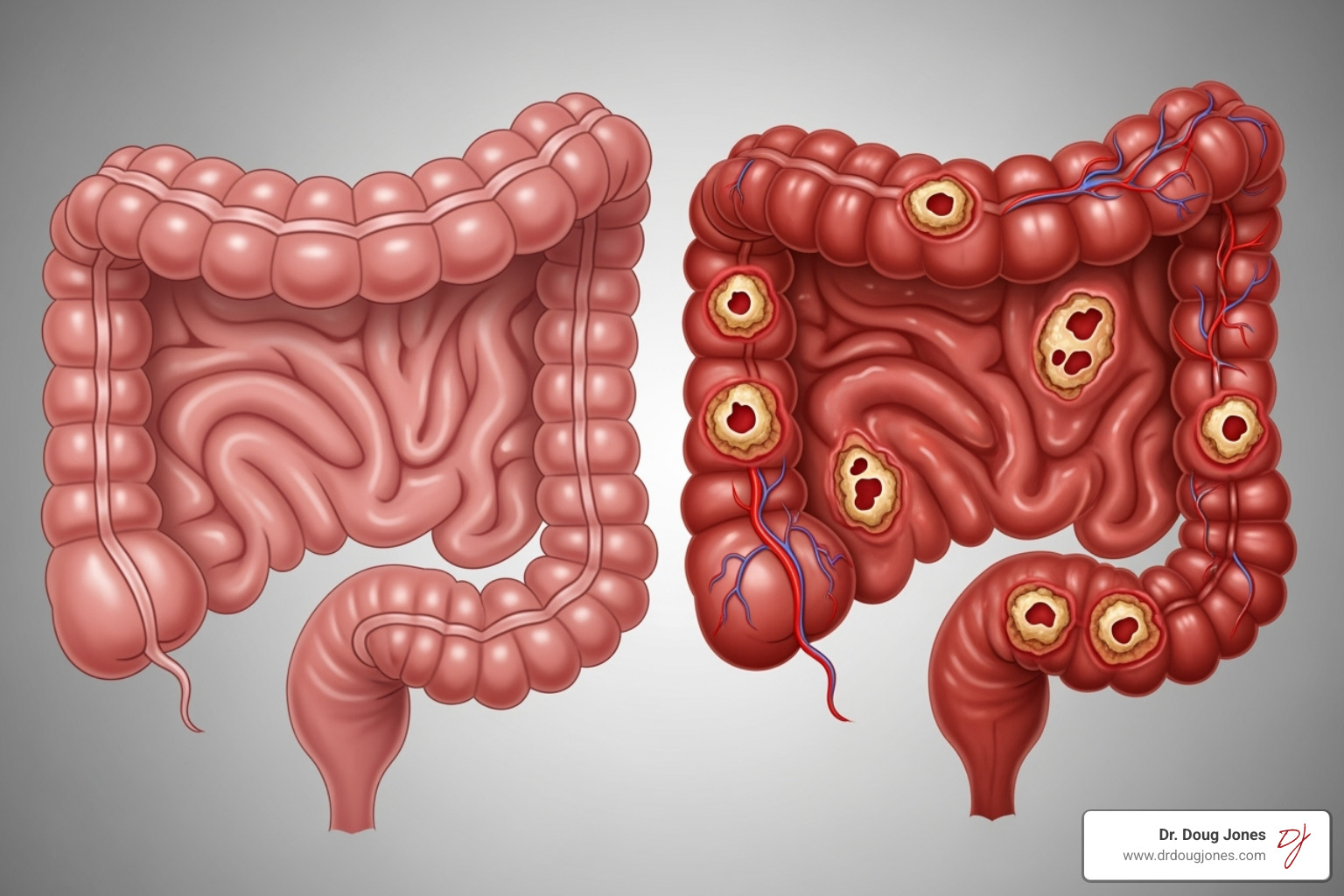
IBD involves widespread intestinal inflammation. It includes two main conditions:
- Crohn's disease can affect any part of the digestive tract, from mouth to anus, in patches. The inflammation goes deep into the bowel wall, causing scarring and narrowing. About one-sixth of patients develop symptoms before age 15.
- Ulcerative colitis is confined to the large intestine and rectum, with continuous inflammation on the inner lining that causes ulcers and bleeding.
Both conditions cause abdominal cramping, chronic diarrhea (often with blood or mucus), unexplained weight loss, and anemia. IBD can also cause symptoms outside the gut, such as joint pain, skin rashes, and eye inflammation, which are known as extraintestinal manifestations.
Celiac Disease: A Reaction to Gluten
In celiac disease, eating gluten (a protein in wheat, barley, and rye) triggers an immune attack on the small intestine. This attack damages the villi—tiny, finger-like projections responsible for nutrient absorption.
This damage, called villous atrophy, leads to malabsorption and inflammation. Common symptoms include chronic bloating, abdominal pain, diarrhea, and constipation. Beyond the gut, celiac disease can cause profound fatigue, iron-deficiency anemia, and an itchy skin rash called dermatitis herpetiformis. The only treatment is a strict, lifelong gluten-free diet, which requires significant lifestyle changes.
Systemic Autoimmune Diseases and Stomach Pain
Some autoimmune diseases are systemic, meaning they affect the entire body, including the digestive tract. This can cause chronic stomach pain that may seem unrelated to the primary diagnosis.
- Systemic Lupus Erythematosus (SLE) can cause lupus enteritis (small intestine inflammation), protein leakage from the intestines, or pancreatitis.
- Systemic sclerosis (scleroderma) causes tissue hardening, leading to digestive issues like esophageal dysmotility (in up to 90% of patients) and gastroparesis (delayed stomach emptying).
- Sjögren's syndrome, known for dry eyes and mouth, can also cause chronic atrophic gastritis and affect the pancreas and liver.
- Other conditions like polyarteritis nodosa, Churg-Strauss syndrome, Henoch-Schönlein purpura, and ankylosing spondylitis can also have significant gastrointestinal manifestations.
These examples show how systemic autoimmunity can create a complex web of symptoms affecting a patient's entire quality of life.
Gastrointestinal Manifestations in Systemic Autoimmune Diseases.
The Path to Diagnosis for an Auto Immune Disorder Chronic Stomach Pain
Diagnosing auto immune disorder chronic stomach pain can be challenging, as symptoms often overlap with more common issues like IBS or acid reflux. Many patients experience shifting symptoms for years before getting answers. A thorough, systematic approach is essential to pinpoint the correct cause.

Key Symptoms and When to See a Doctor
While occasional stomach upset is normal, certain persistent warning signs may indicate an autoimmune attack on your digestive system. See a doctor if you experience:
- Persistent abdominal pain that doesn't resolve with simple remedies.
- Unexplained weight loss, which can signal poor nutrient absorption.
- Chronic diarrhea or constipation lasting for weeks.
- Severe fatigue that isn't relieved by rest.
- Symptoms of anemia, such as pale skin, shortness of breath, or dizziness.
- New neurological symptoms like tingling in the hands or feet, balance issues, or memory problems, which could indicate B12 deficiency.
Experiencing several of these symptoms for more than a few weeks warrants a comprehensive medical evaluation.
Diagnostic Process for Autoimmune-Related Stomach Pain
The diagnostic process involves a detailed health history, physical exam, and specific tests:
- Blood Tests: A Complete Blood Count (CBC) checks for anemia, while inflammatory markers (CRP, ESR) measure inflammation. Specific autoantibody tests help identify conditions like celiac disease (tTG-IgA) or autoimmune gastritis (anti-parietal cell and anti-intrinsic factor antibodies).
- Nutrient Level Testing: We check levels of Vitamin B12, iron, and ferritin to assess for malabsorption.
- Endoscopy and Colonoscopy: These procedures use a camera to view the digestive tract. A biopsy, where a small tissue sample is taken, is the gold standard for confirming a diagnosis by revealing microscopic changes characteristic of specific autoimmune conditions.
This comprehensive approach ensures an accurate diagnosis and an effective treatment plan.
A Functional Approach to Managing Autoimmune Stomach Pain
A diagnosis for auto immune disorder chronic stomach pain is the first step. A functional approach looks at the whole picture, addressing the root causes that keep the immune system overactive, rather than just treating symptoms.

Foundational Medical Treatments
Medical treatments often form a necessary foundation for healing:
- Condition-specific treatments: These target the particular autoimmune condition, such as biologic therapies for IBD or a strict gluten-free diet for celiac disease.
- Nutrient repletion: This is critical for correcting deficiencies caused by malabsorption. Examples include lifelong B12 injections for autoimmune gastritis or iron infusions for severe anemia.
- Immunosuppressive medications: These can be used to calm an overactive immune system, giving the gut a chance to heal.
Lifestyle and Dietary Strategies for Managing Autoimmune-Related Stomach Pain
Your daily choices are powerful tools for managing auto immune disorder chronic stomach pain:
- Anti-inflammatory diet: Focus on whole foods like colorful vegetables, fruits, lean proteins, and healthy fats (olive oil, avocado, fatty fish). Introduce fiber slowly to support gut health.
- Identifying food triggers: An elimination diet, guided by a professional, can help pinpoint foods that worsen inflammation. Common triggers include dairy, soy, and corn.
- Stress management: Chronic stress can inflame the gut. Practices like yoga, meditation, and deep breathing are essential for healing the gut-brain connection.
- Supporting your gut microbiome: Nurture beneficial gut bacteria with probiotics (supplements) and prebiotics (foods like garlic, onions, and asparagus).
The Importance of Long-Term Monitoring
Managing an autoimmune condition is a long-term partnership with your healthcare team to optimize health and prevent problems.
- Regular follow-ups: Seeing your gastroenterologist and immunologist allows for treatment adjustments and early detection of changes.
- Monitoring for complications: This includes regular blood tests to check for nutritional deficiencies and screening for the slightly increased cancer risk associated with some conditions.
- Endoscopic surveillance: For conditions like AAG and IBD, periodic endoscopy or colonoscopy is crucial for spotting precancerous changes early. For AAG, this may be every one to five years, depending on the findings.
This proactive approach helps you manage the disease and optimize your immune health for the long haul.
Frequently Asked Questions about Autoimmune Stomach Pain
When you're dealing with auto immune disorder chronic stomach pain, it's natural to have questions about what's happening in your body and how different factors might affect your symptoms. Let me address some of the most common concerns I hear from patients in my practice.
Can stress cause or worsen an autoimmune stomach flare-up?
Yes, absolutely. The gut-brain axis is a direct communication line between your brain and digestive system. When you're stressed, your body releases hormones like cortisol that increase inflammation, which can worsen an auto immune disorder chronic stomach pain flare-up. This is why stress management—through practices like yoga, meditation, or deep breathing—is a cornerstone of any effective treatment plan. It's not just in your head; it's a physiological response.
Is Irritable Bowel Syndrome (IBS) an autoimmune disease?
IBS is not an autoimmune disease; it is a functional disorder. This means the gut isn't working correctly, but there is no immune-mediated tissue damage as seen in conditions like IBD or celiac disease. In IBS, the gut appears normal on examination.
However, the symptoms of IBS—abdominal pain, bloating, and altered bowel habits—can overlap significantly with autoimmune conditions. This makes proper diagnostic testing crucial to distinguish between them, as treatment is very different. It is also possible to have both an autoimmune condition and IBS concurrently.
What is the difference between autoimmune gastritis and H. pylori gastritis?
The key difference is the cause of inflammation. In autoimmune gastritis, the body's own immune system attacks the stomach lining. In H. pylori gastritis, the inflammation is caused by the Helicobacter pylori bacteria.
While symptoms like stomach pain and bloating can be similar, treatments are entirely different. H. pylori gastritis is treated with antibiotics, whereas autoimmune gastritis requires managing the immune response and correcting nutrient deficiencies (like B12).
Interestingly, a chronic H. pylori infection can sometimes trigger autoimmune gastritis in predisposed individuals. The infection may confuse the immune system, causing it to attack the stomach's own cells. This highlights why an accurate diagnosis is essential for effective treatment.
Conclusion: Taking Control of Your Immune and Digestive Health
Struggling with persistent stomach pain is a common experience for millions, and it can be a sign of an underlying autoimmune condition. As we've discussed, conditions like autoimmune gastritis, IBD, celiac disease, and systemic disorders occur when the body's defense system mistakenly attacks the gut.
Understanding this connection is the first step toward feeling better. It empowers you to seek a proper diagnosis through specific blood tests, endoscopy, and biopsies. While the path to diagnosis can be frustrating, it is essential for effective treatment.
Lasting relief comes from a comprehensive management plan that combines medical treatments (like nutrient repletion or biologics) with personalized lifestyle strategies. This includes an anti-inflammatory diet, stress management, and ongoing monitoring to prevent complications.
At GAIN, we specialize in these complex immune challenges. Our goal is to empower you with the knowledge and personalized care needed to move from feeling helpless to becoming an active partner in your health. Your immune system is unique, and your treatment plan should be too.
If you suspect an autoimmune connection to your chronic stomach pain, don't wait. Addressing the root cause early is key to better long-term health.
Learn more about our personalized approach to immune health.

