Beyond the Acute: Navigating Life as a COVID Long Hauler
Are you a COVID long hauler? Discover common symptoms, effective management strategies, and vital support for your recovery journey.

Understanding What It Means to Be a COVID Long Hauler

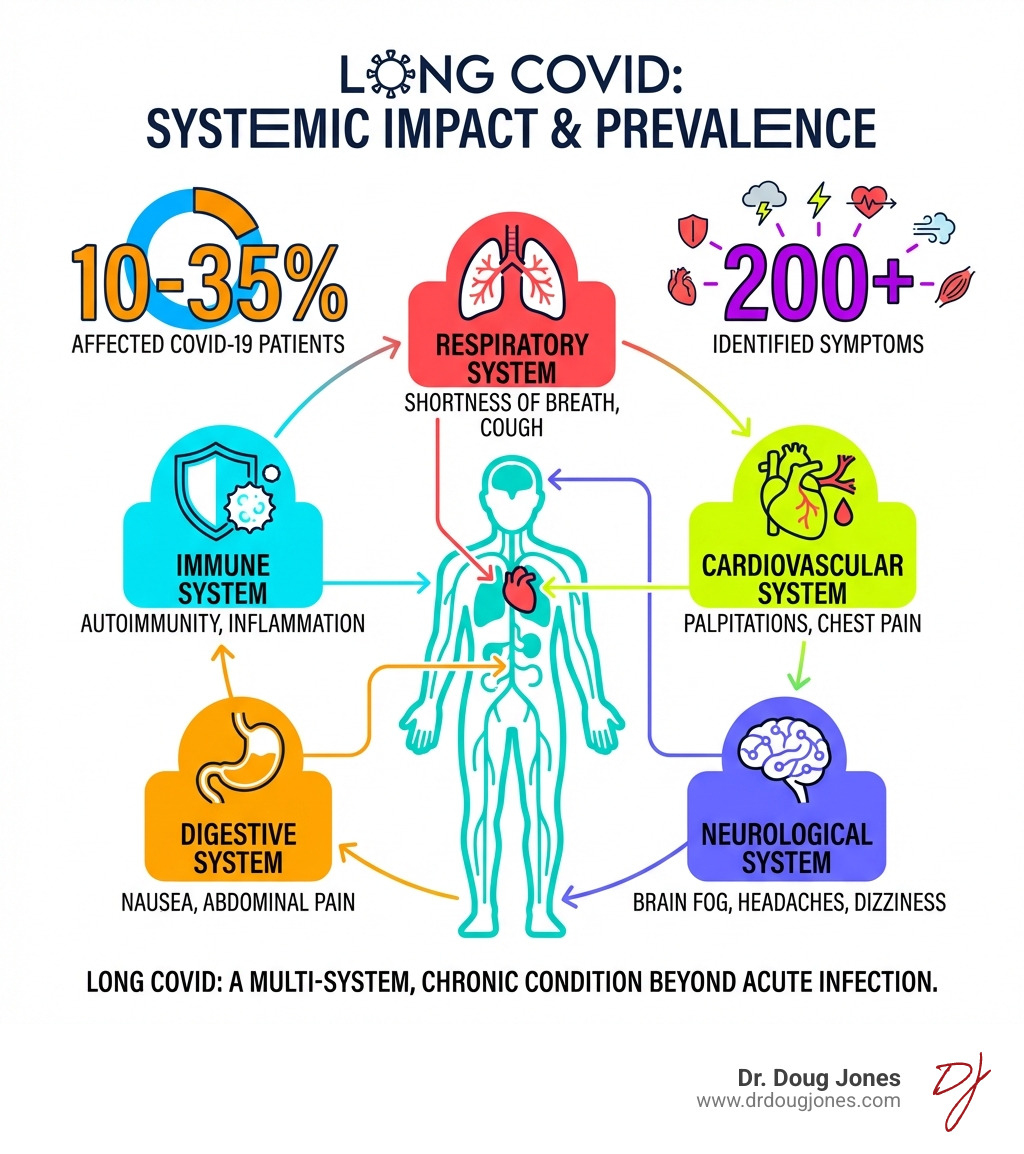
A COVID long hauler is someone who experiences ongoing symptoms weeks, months, or even years after their initial COVID-19 infection has resolved. This condition—officially called Long COVID or Post-COVID Conditions—affects millions of people worldwide and can impact nearly every organ system in the body.
Key Facts About COVID Long Haulers:
- Definition: Symptoms that persist or develop at least 3 months after COVID-19 infection
- Prevalence: Researchers estimate 10-35% of people who had COVID-19 develop Long COVID
- Symptom Count: More than 200 different symptoms have been identified
- Duration: Symptoms can last weeks, months, or years and may come and go
- Who's Affected: Anyone can become a long hauler, regardless of initial illness severity
- Most Common Symptoms: Fatigue, brain fog, post-exertional malaise, shortness of breath, heart palpitations
Long COVID is not a single illness. It's a chronic condition that can affect multiple organ systems simultaneously. The symptoms may improve over time, worsen unexpectedly, or persist unchanged. Some people develop new health conditions like diabetes, POTS, or heart problems as a result.
What makes this especially challenging is that there's no single test to diagnose Long COVID. Many people face dismissal from healthcare providers or struggle to get their symptoms validated, especially when routine blood work and imaging come back normal.
As a board-certified immunologist who specializes in complex immune conditions including COVID long hauler syndrome, I've worked with countless patients navigating this difficult journey. My approach focuses on understanding the underlying immune dysregulation and helping patients regain control of their health through comprehensive, evidence-based care.
What is Long COVID? Understanding the Basics
When we talk about Long COVID, we're referring to a complex, chronic condition that lingers long after the initial SARS-CoV-2 infection has passed. It's not just a prolonged recovery from a bad flu; it's a distinct health challenge that can dramatically alter a person's life.
Defining Post-COVID Conditions
The official term for Long COVID is Post-COVID Conditions (PCC). It's defined as a chronic condition that arises after SARS-CoV-2 infection and is present for at least 3 months. These symptoms can be continuous, they can come and go (relapsing and remitting), or they can progressively worsen. Importantly, they affect one or more organ systems and cannot be explained by other health problems.
The World Health Organization (WHO) has also developed a definition for post-COVID-19 condition, which aligns with this understanding: it encompasses coronavirus symptoms that persist or return three months after a person becomes ill from infection with SARS-CoV-2, impacting daily functioning. This consistent definition helps healthcare providers and researchers speak the same language when addressing this multifaceted condition. You can read the WHO definition of post-COVID-19 condition for more details.
The Leading Theories Behind Long-Term Symptoms
Why does COVID-19 lead to such long-term health problems? Researchers are actively exploring several theories, and it's likely a combination of these factors contributes to the diverse experiences of COVID long haulers.
One prominent theory involves organ damage from the acute infection. Even mild cases of COVID-19 can cause subtle damage to various organs, leading to lasting issues. Another key factor is persistent inflammation or a dysregulated inflammatory state. Our immune system, which is designed to protect us, can sometimes go into overdrive or become imbalanced after an infection. For more on how your body's defenses work, check out More info about your immune system.
Other theories include:
- Microvascular dysfunction: Problems with the smallest blood vessels, affecting blood flow and oxygen delivery to tissues.
- Ongoing viral activity or viral reservoir: The virus might persist in some parts of the body, continuing to cause issues.
- Autoimmunity: The immune system might mistakenly attack healthy cells and tissues after the infection, leading to autoimmune conditions. This is a bit like When Your Immune System Acts Like a Smoke Alarm, where it's reacting strongly even when the initial threat is gone.
- Inadequate antibody response: Some people might not develop a strong enough or appropriate antibody response, leaving them vulnerable to ongoing problems.
- Gut microbiome disruption: The balance of bacteria in the gut can be significantly altered, impacting overall health and immunity.
How Long Can Symptoms Last and What is the Recovery Timeline?
This is often one of the most frustrating questions for a COVID long hauler: "How long will this last?" The answer is, unfortunately, highly variable. Long COVID symptoms can persist for weeks, months, or even years after the initial infection.
While some people experience significant improvement within 3 to 6 months, others find their symptoms continue far longer. The journey is rarely linear; symptoms can emerge, persist, resolve, and then re-emerge, creating a rollercoaster of health. This fluctuating nature makes it difficult to predict a typical recovery timeline. Each individual's path is unique, influenced by their own body's response and the specific constellation of symptoms they experience.
Identifying the Symptoms of a COVID Long Hauler
The sheer number and variety of symptoms associated with Long COVID are astounding. More than 200 different symptoms have been identified, affecting virtually every part of the body. This is why it's often described as a multi-system condition, impacting multiple organs and body functions simultaneously.
The Most Common Symptoms You Shouldn't Ignore
While the list is extensive, some symptoms are more commonly reported by COVID long haulers. These are the ones we hear about most frequently and often have the biggest impact on daily life:
- Fatigue: This isn't just regular tiredness; it's a profound, debilitating exhaustion that isn't relieved by rest. It can make even simple tasks feel monumental.
- Brain fog: Difficulty concentrating, memory problems, confusion, and slowed thinking are hallmarks of Long COVID. It can feel like your brain is wading through mud.
- Post-Exertional Malaise (PEM): This is a critical symptom where physical or mental exertion leads to a significant worsening of symptoms, often 12 to 48 hours later, and can last for days or weeks. It's a key indicator of energy envelope dysfunction.
- Shortness of breath: Persistent breathlessness, even at rest or with minimal activity, can be alarming.
- Heart palpitations: A feeling of a racing, pounding, or fluttering heart, often accompanied by chest pain.
- Headaches: Chronic or recurring headaches, sometimes severe and unlike previous headaches.
- Loss of smell or taste: While often an early symptom of acute COVID-19, it can persist for months or even become distorted (parosmia). Good news is, studies suggest 60% to 80% see improvement within a year, and 95% eventually recover these senses, though it might take a while!
- Sleep problems: Insomnia, unrefreshing sleep, or disrupted sleep patterns are common.
- Muscle and joint pain: Aches and pains throughout the body that can be persistent and migratory.
- Dizziness or lightheadedness: Especially when standing up, often linked to conditions like POTS.
- Gastrointestinal issues: Diarrhea, constipation, stomach pain, or nausea.
- Mental health impacts: Anxiety, depression, and even symptoms of post-traumatic stress disorder (PTSD) are frequently reported.
How Long COVID Affects Multiple Organ Systems
COVID-19 is far more than a respiratory illness. It can affect virtually every organ system in the body, leading to a wide array of symptoms for COVID long haulers:
- Lungs: Persistent cough, shortness of breath, and reduced lung capacity due to damage to lung tissue.
- Heart: Myocarditis (inflammation of the heart muscle), palpitations, irregular heartbeat, and increased risk of heart failure. One study even found 60% of recovered patients had signs of ongoing heart inflammation.
- Brain & Neurological System: Brain fog, headaches, dizziness, nerve pain (pins-and-needles), altered smell/taste, and even tremors. The virus can directly impact the nervous system or cause inflammation that affects brain function.
- Kidneys: Acute kidney injury during the initial infection can lead to long-term kidney dysfunction.
- Liver: Liver inflammation and damage have been observed.
- Skin: Rashes, hair loss, and changes in skin color or texture.
- Vascular System: Increased risk of blood clots, which can lead to serious complications like stroke or pulmonary embolism.
- Endocrine System: Disruption of hormone regulation, potentially affecting blood sugar control.
New Health Complications That Can Arise
Beyond the direct symptoms, Long COVID can also trigger the development of new medical conditions or worsen existing ones. This is a significant concern for COVID long haulers and their healthcare providers:
- Diabetes: Some individuals develop new-onset type 2 diabetes or experience worsening control of pre-existing diabetes after COVID-19.
- Heart conditions: Beyond inflammation, long-term heart issues like arrhythmias or heart failure can emerge.
- Blood clots: The risk of dangerous blood clots can persist, leading to conditions like deep vein thrombosis or pulmonary embolism.
- Neurological conditions: Long-term cognitive impairment, chronic headaches, and other neurological disorders can develop.
- Postural Orthostatic Tachycardia Syndrome (POTS): This is a common post-COVID complication characterized by an abnormal increase in heart rate upon standing, leading to dizziness, fatigue, and brain fog.
- Post-Intensive Care Syndrome (PICS): For those who experienced severe COVID-19 and spent time in the ICU, PICS can contribute to long-term physical weakness, cognitive problems, and psychological issues like PTSD. PICS isn't exclusive to COVID-19, but it can certainly overlap with and exacerbate Long COVID symptoms. You can learn More about post-intensive care syndrome (PICS).
Diagnosis, Risk Factors, and Prevention
Navigating Long COVID can feel like trying to solve a mystery without all the clues. The diagnostic process is still evolving, and understanding who is most at risk, and how to prevent it, are crucial pieces of the puzzle.

How Doctors Diagnose a COVID Long Hauler
A challenge for a COVID long hauler is the lack of a definitive diagnostic test. There isn't a simple blood test or imaging scan that can unequivocally say, "Yes, this is Long COVID." Instead, diagnosis is a clinical process, relying heavily on:
- Patient history: A thorough account of your symptoms, their onset, duration, and their impact on your daily life, crucially noting a prior COVID-19 infection (confirmed by test, symptoms, or exposure).
- Physical examination: A comprehensive check-up to assess your overall health and specific symptoms.
- Ruling out other conditions: Doctors will perform various tests (blood work, organ function tests, imaging) to ensure your symptoms aren't caused by another underlying health issue. This is a vital step, even if the results come back "normal," as objective lab findings don't always capture the full picture of Long COVID.
The good news is that Post-COVID Condition was incorporated into the International Classification of Diseases (ICD-10-CM) as code U09.9 as of October 1, 2021. This means healthcare providers have a way to officially document the condition, which is important for both patient care and public health surveillance.
It's common for patients to feel dismissed or unheard when their tests return normal, yet they continue to suffer. If you find yourself in this situation, your experience is valid, and there are Tips for when you don't feel heard by your doctor.
Are You at Higher Risk?
While anyone who gets COVID-19 can become a COVID long hauler, some factors increase the likelihood:
- Severity of initial illness: People who had severe COVID-19, especially those hospitalized or in the ICU, are more prone to Long COVID. However, even mild or asymptomatic cases can lead to long-term symptoms.
- Female sex: Studies consistently show that women are more likely to develop Long COVID than men.
- Underlying health conditions: Individuals with pre-existing conditions like diabetes, heart disease, or autoimmune disorders may be at higher risk.
- Unvaccinated status: Not getting a COVID-19 vaccine is a significant risk factor for developing Long COVID.
- Age: Adults 65 and older also face a higher risk.
- Reinfection: Getting reinfected with SARS-CoV-2 increases the risk of developing Long COVID.
Health inequities also play a role, with certain demographic groups, such as Hispanic and Latino people, experiencing disproportionately higher rates.
The Role of COVID-19 Vaccines in Prevention
One of the most powerful tools we have against Long COVID is vaccination. Research indicates that COVID-19 vaccines can significantly help prevent Long COVID.
The vaccines reduce the risk of initial infection, and if a breakthrough infection occurs, they typically lead to a milder illness, which in turn lowers the risk of developing long-term symptoms. Studies have shown that vaccinated individuals who get COVID-19 have a decreased chance of becoming a COVID long hauler compared to unvaccinated individuals. This protective effect extends to children as well. Staying up to date with COVID-19 vaccinations and boosters is one of the best proactive steps you can take to protect yourself and your family from becoming a long hauler.
Managing Long COVID and Finding a Path to Recovery
Living as a COVID long hauler often means adapting to a new normal, where energy levels, cognitive function, and physical abilities can be unpredictable. The good news is that management strategies are evolving, focusing on symptom relief, rehabilitation, and improving overall quality of life.
Current Treatment and Symptom Management Strategies
Since Long COVID presents with such a wide array of symptoms, treatment is highly individualized and symptom-based. There's no one-size-fits-all cure, but rather a focus on managing each specific issue. This often involves a multidisciplinary care team, which might include neurologists, cardiologists, pulmonologists, physical therapists, occupational therapists, and mental health professionals.
Key strategies include:
- Physical therapy: For muscle weakness, pain, and improving overall function.
- Pacing for PEM: Learning to manage energy levels and avoid overexertion to prevent symptom crashes. This involves carefully balancing activity and rest.
- Cognitive rehabilitation: Exercises and strategies to improve brain fog, memory, and concentration.
- Mental health support: Addressing anxiety, depression, PTSD, and the emotional toll of chronic illness is crucial. You can find Information on managing mental health symptoms from government health agencies.
- Medications and supplements: Prescribed to alleviate specific symptoms like pain, sleep disturbances, or heart rate irregularities.
- Olfactory training: For loss of smell, though its effectiveness is still being studied.
At Dr. Doug Jones, we believe in Personalized Care Solutions that consider your unique symptoms and needs, creating a custom management plan to optimize your function and well-being.
The Overlap with ME/CFS and Other Chronic Illnesses
Many COVID long haulers find their symptoms strikingly similar to other chronic conditions, particularly Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). This overlap is significant, as understanding these similarities can inform treatment approaches and patient experience. Other conditions with similar symptom profiles include Fibromyalgia and Dysautonomia.
| Feature | Long COVID (PCC) | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) |
|---|---|---|
| Trigger | SARS-CoV-2 infection | Often post-viral infection (e.g., Epstein-Barr), but can be non-infectious or have an unknown trigger. |
| Core Symptom | Post-Exertional Malaise (PEM) is a key feature for many, but not all. | Post-Exertional Malaise (PEM) is a mandatory hallmark symptom for diagnosis. |
| Shared Symptoms | Profound fatigue, brain fog, unrefreshing sleep, muscle/joint pain, headaches, dizziness (POTS), sore throat. | Profound fatigue, brain fog, unrefreshing sleep, muscle/joint pain, headaches, dizziness (POTS), sore throat. |
| Diagnosis | Clinical diagnosis based on symptoms persisting >3 months post-COVID, after ruling out other causes. | Clinical diagnosis based on established criteria (e.g., IOM criteria), requiring symptoms for at least 6 months, after ruling out other causes. |
The diagnostic difficulties and shared symptoms highlight the complexity of these post-viral illnesses. You can Learn more about ME/CFS from advocacy and research organizations.
