Beyond the Sniffles: Locating a Top Food Allergy Doctor
Conquer food allergy anxiety. Find a top food allergy doctor for expert diagnosis, modern treatment, and a path to better living.

Why Finding the Right Food Allergy Doctor Changes Everything

A food allergy doctor is a board-certified allergist and immunologist who specializes in diagnosing and treating food allergies using methods like patient history, skin prick tests, blood tests, oral food challenges, and personalized treatment plans including avoidance strategies, emergency preparedness, and emerging therapies like Oral Immunotherapy (OIT), sublingual immunotherapy (SLIT), and biologics.
Quick Guide: What to Look For in a Food Allergy Doctor
- Board certification in Allergy and Immunology
- Comprehensive diagnostic approach using history, skin tests, blood work, and food challenges
- Treatment options beyond strict avoidance, including OIT, SLIT, and biologics when appropriate
- Emergency planning with epinephrine training and anaphylaxis action plans
- Long-term partnership for quality of life improvement and ongoing management
Food allergies are a growing concern, with prevalence in children increasing significantly over the past two decades. The economic cost is staggering, but the true burden is the daily anxiety and social limitations that impact families.
Anaphylaxis, a severe allergic reaction, leads to thousands of ER visits annually. With a limited number of specialists available, finding the right one can feel overwhelming.
But here's the truth: the right food allergy doctor doesn't just manage symptoms—they help you reclaim your life. Whether you're navigating a new diagnosis, seeking treatment options beyond avoidance, or dealing with persistent reactions that other doctors haven't been able to pinpoint, expert care makes all the difference.
The field is evolving rapidly. Oral immunotherapy is showing high success rates in desensitizing patients. Early allergen introduction is preventing allergies before they start. And allergists are moving from a purely cautious approach to one that empowers patients and families to actively manage—and sometimes overcome—food allergies.
I'm Dr. Doug Jones, a board-certified immunologist who has spent over a decade helping patients steer complex food allergies and immune challenges. As a food allergy doctor, I've seen how the right diagnosis and treatment approach can transform not just health outcomes, but entire family dynamics. In this guide, I'll walk you through exactly how to find, work with, and benefit from a top food allergy specialist.
Step 1: Understanding Your Symptoms and When to See a Specialist
Understanding the signs your body is sending is the first crucial step toward effective food allergy management. Many symptoms can be vague or mimic other conditions, making accurate diagnosis by a food allergy doctor essential. The immune system is a complex beast, and when it misidentifies a harmless food protein as a threat, chaos can ensue.

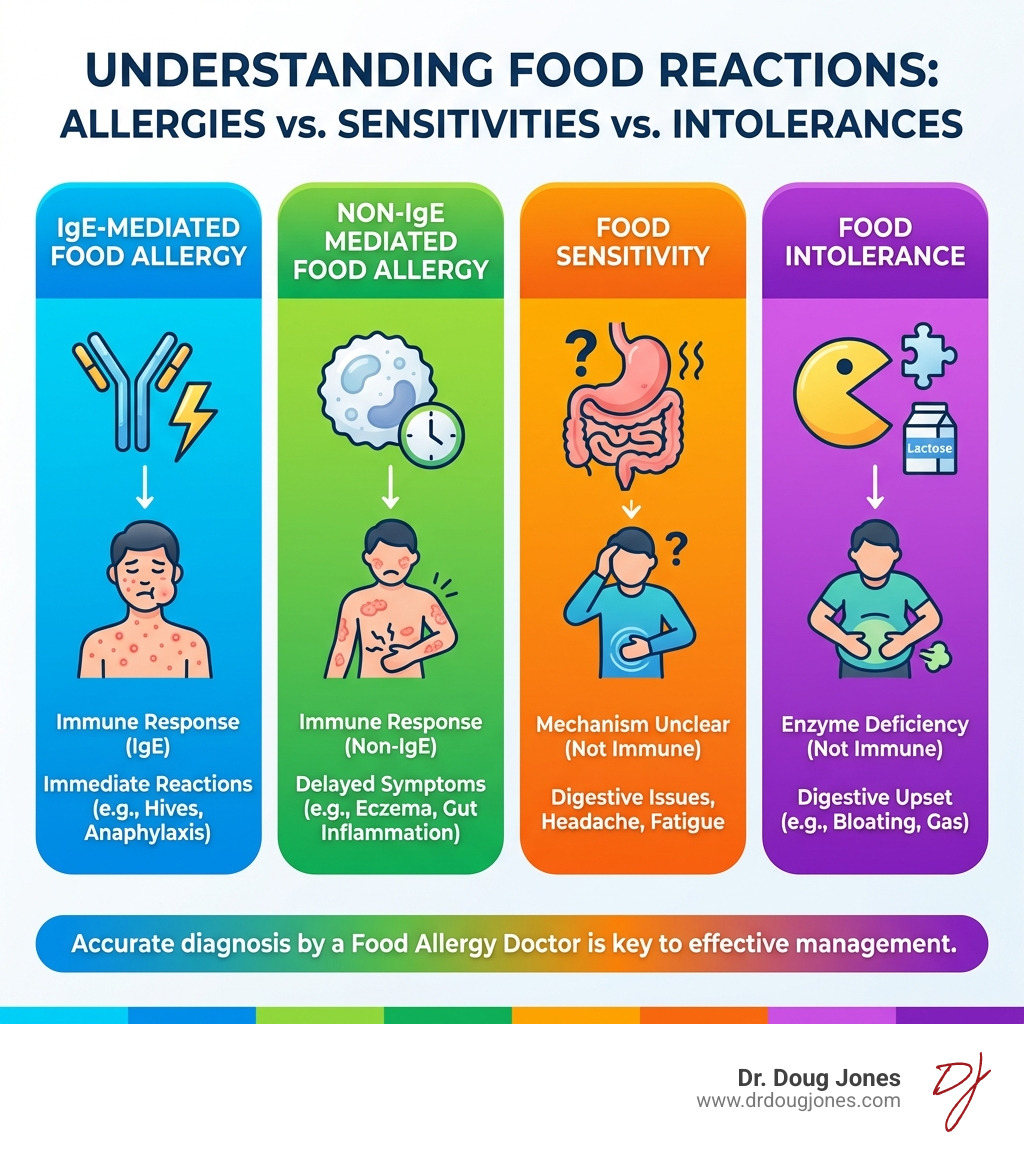
Generally, food allergies fall into two main categories based on the immune response:
- IgE-mediated allergies: These are the most common and often the most severe, involving immunoglobulin E (IgE) antibodies. Reactions are typically rapid, occurring within minutes to a couple of hours after exposure.
- Non-IgE-mediated allergies: These involve other parts of the immune system and don't produce IgE antibodies. Reactions are usually delayed, sometimes appearing hours or even days after eating the culprit food. Symptoms often affect the gastrointestinal tract. They can be life-threatening as in the case of food protein-induced enterocolitis syndrome (FPIES) or non-life-threatening, yet chronic and potentially debilitating like eosinophilic esophagitis (EoE).
The "Top 9" common food allergens are responsible for the vast majority of allergic reactions, but any food can potentially trigger one. Recognizing the signs and understanding the difference between a true allergy and a food intolerance or sensitivity is paramount. Only a true food allergy involves a specific immune response. To learn more about these distinctions, check out What's the difference between allergies and intolerances?.
The development of food allergies is a complex interplay of genetics and environmental factors. The dramatic rise in prevalence suggests that our modern environment plays a significant role. Factors like gut microbiome composition have been linked to asthma and food allergy in children, hinting at the intricate connections within our bodies. Understanding the underlying mechanisms is key to addressing The root cause of allergies.
Common Types of Food Allergies and Their Symptoms
While reactions vary, they are most often caused by the 'Top 9' allergens: milk, eggs, peanuts, tree nuts, soy, wheat, fish, shellfish, and sesame. Symptoms can affect multiple body systems and include:
- Skin reactions: Hives, eczema flare-ups, swelling (angioedema) of the lips, face, or throat.
- Respiratory symptoms: Wheezing, shortness of breath, coughing, or nasal congestion.
- Gastrointestinal issues: Nausea, vomiting, diarrhea, or abdominal pain.
- Cardiovascular symptoms: Dizziness, fainting, weak pulse, or a drop in blood pressure (signs of anaphylaxis).
The "Atopic March": Connecting Eczema, Food Allergies, and Asthma
Have you ever noticed that many children with food allergies also have eczema, or later develop asthma? This common progression is known as the "Atopic March."
Research shows a link between infant eczema and a higher risk of developing food allergies. A compromised skin barrier may allow allergens to penetrate the skin, sensitizing the immune system. This insight has revolutionized allergy prevention, shifting focus from delaying to early introduction of common allergens under medical supervision to promote tolerance.
The Atopic March doesn't stop there. Children with food allergies also have an increased risk for developing asthma and allergic rhinitis. This interconnectedness underscores the importance of a holistic approach, where a food allergy doctor considers the entire allergic profile of a patient. For instance, some individuals might experience eosinophilic esophagitis, an allergic condition affecting the esophagus, which is part of this broader allergic spectrum. You can find More on Eosinophilic Esophagitis Treatment and how it fits into comprehensive allergy care.
Step 2: What to Expect During Diagnosis with a Top Food Allergy Doctor
When you suspect a food allergy, consulting a board-certified allergist is the best course of action. These specialists, often called a food allergy doctor, are uniquely qualified to solve the complexities of your immune system.

The diagnostic journey is rarely a one-size-fits-all process. It begins with a thorough evaluation, because no single test can definitively confirm a food allergy. This comprehensive approach is what sets expert care apart. For a deeper dive into the diagnostic process, explore Food Allergy Testing 101.
Preparing for your appointment can make a big difference. We encourage you to watch this Helpful video on preparing for your allergist appointment to make the most of your visit.
How a food allergy doctor uses your history for diagnosis
Your story is perhaps the most powerful diagnostic tool a food allergy doctor has. We will listen intently to your experiences to guide our diagnostic strategy. Expect to discuss:
- Symptom details: A detailed description of all symptoms (skin, respiratory, etc.).
- Timing and context: How quickly symptoms appeared after eating, what foods were consumed, and in what quantity.
- Co-factors: Whether you were exercising, stressed, or taking medications.
- Personal and family history: Any personal or family history of allergies, asthma, or eczema.
A crucial part of this process is ensuring you feel heard. Your insights are invaluable. If you've ever felt dismissed in a medical setting, these 8 tips for when you don't feel heard by your doctor can help you advocate for yourself.
Key Diagnostic Tests Explained
After gathering your history, your food allergy doctor may recommend specific tests to support the clinical picture.
- Skin Prick Test (SPT): A small drop of a liquid food allergen is placed on your skin, which is then gently pricked. After 15-20 minutes, the site is observed for a raised, red, itchy bump (a wheal). A positive result indicates the presence of IgE antibodies, suggesting a potential allergy, but it doesn't always mean a clinical allergy exists.
- Blood Test (Specific IgE): This test measures the amount of IgE antibodies to specific foods in your blood. Higher levels can indicate a higher likelihood of an allergy, but like SPTs, a positive test alone isn't enough for a diagnosis. If someone is offering IgG testing as "sensitivity" or "intolerance" tests, then they are likely not a specialist and you may consider seeking a second opinion as they are recommending non-validated tests.
- Oral Food Challenge (OFC): Often considered the "gold standard" for diagnosis, an OFC involves consuming gradually increasing amounts of the suspected food under strict medical supervision. This allows the food allergy doctor to observe for any reactions in a controlled setting. OFCs should never be attempted at home.
Understanding these results can be complex. Our article on How to read food allergy results without panic offers valuable insights.
Step 3: Exploring Modern Treatment Options Beyond Avoidance
For decades, the primary management strategy for food allergies was strict avoidance of the allergen and carrying an epinephrine auto-injector for emergencies. While avoidance remains a cornerstone, a food allergy doctor today can offer a broader spectrum of approaches.
Complete avoidance, while seemingly safe, comes with significant limitations. It requires constant vigilance, meticulous label reading, and an acute awareness of cross-contamination risks. This burden can lead to considerable anxiety and social limitations.
The critical importance of emergency preparedness cannot be overstated. Anaphylaxis is a severe reaction that requires immediate attention. This means always carrying an epinephrine auto-injector (such as an EpiPen®) and having a clear Anaphylaxis Emergency Plan. We strongly recommend visiting EpiPen® information for crucial details on how to use this life-saving device. Your food allergy doctor will ensure you and your family are thoroughly trained in its use.
Thankfully, the landscape of food allergy treatment is evolving. We are entering A New Era in Food Allergy Treatment that offers hope beyond just avoidance.
Oral Immunotherapy (OIT): A Path to Desensitization
One of the most exciting advancements is Oral Immunotherapy (OIT). This approach aims to desensitize patients to their food allergens, improving their quality of life and providing a safety net against accidental exposures.
What is OIT? OIT involves giving a person with a food allergy tiny, increasing doses of the food they are allergic to, under strict medical supervision. The goal is to gradually retrain the immune system to tolerate the allergen.
How OIT works: The process starts with a controlled initial dose in a clinical setting. Subsequent doses are taken daily at home, with periodic visits to the food allergy doctor for dose escalations. Over time, the immune system becomes less reactive.
Desensitization vs. Tolerance: OIT typically achieves desensitization, which means the patient can tolerate a certain amount of the allergen as long as they continue daily treatment. This provides a safety net against accidental exposure. A less common but sometimes achievable outcome is sustained unresponsiveness (true tolerance), where the food can be eaten freely even after stopping treatment. Studies show high success rates in desensitizing patients. For insights into the long-term safety and outcomes of OIT, refer to this Scientific research on long-term OIT safety.
Patient eligibility: OIT is not for everyone. It requires a significant commitment and carries risks. Your food allergy doctor will carefully assess your medical history, allergy profile, and lifestyle to determine if OIT is a suitable option.
Here's a quick comparison of the traditional avoidance approach versus OIT:
| Feature | Strict Avoidance | Oral Immunotherapy (OIT) |
|---|---|---|
| Goal | Prevent all reactions | Desensitize to prevent reactions from accidental exposure; potentially enable consumption |
| Risk of Reaction | High with accidental exposure | Managed risk during treatment; reduced risk from accidental exposure post-desensitization |
| Daily Burden | High (constant vigilance, label reading) | High during treatment phase (daily dosing); significantly reduced post-desensitization |
| Quality of Life | Often limited by fear and social restrictions | Improved freedom, reduced anxiety, broader dietary choices |
| Emergency Meds | Always required | Always required, but risk of use may decrease |
| Commitment | Lifelong vigilance | Intensive initial phase, ongoing maintenance |
The role of your food allergy doctor in creating a management plan
Your food allergy doctor is your most important partner in this journey. Their role extends far beyond diagnosis; they are essential in crafting a personalized, comprehensive management plan.
This plan involves:
- Personalized treatment: Tailoring strategies based on your specific allergies, reaction history, and lifestyle. This might include avoidance, OIT, or other emerging therapies. We are committed to personalized allergy care for every patient.
- Shared decision-making: Ensuring you are fully informed about all options, risks, and benefits to make choices that align with your values.
- Risk assessment: Continually evaluating your risk of severe reactions and adjusting the management plan as needed.
- Emergency preparedness: Providing thorough training on epinephrine auto-injector use and creating a detailed Anaphylaxis Emergency Plan.
- Regular follow-ups: Monitoring your progress, re-evaluating allergies, and addressing any new concerns.
Step 4: Partnering with Your Allergist for Long-Term Management and Quality of Life
Living with food allergies is a marathon, not a sprint. The ongoing support from your food allergy doctor is invaluable for long-term management and improving your quality of life. This partnership helps transform a life dictated by fear into one of informed confidence.
Effective daily life management involves several key areas:
- Label reading and cross-contamination: Mastering label reading to spot hidden allergens and learning safe food handling practices at home and when dining out.
- School and travel planning: Creating safety plans for school, childcare, and travel by collaborating with staff and providers.
- Psychosocial support and anxiety reduction: Addressing the emotional toll of food allergies, such as anxiety and hypervigilance, through coping strategies and professional support. Our articles on the emotional load of food allergy hypervigilance and navigating holidays with food allergies offer further support.
Finding Reliable Resources and Support
You don't have to face food allergies alone. A strong support network and access to reliable information are vital. Your food allergy doctor can guide you to reputable resources:
- Patient advocacy groups: Organizations like Food Allergy Canada (see their resources here) provide a wealth of information, support networks, and advocacy efforts.
- Online communities: Connecting with others who share similar experiences can offer practical tips and emotional support, but always vet information with your medical team.
- Nutritionist collaboration: A registered dietitian specializing in food allergies can provide invaluable guidance on maintaining a balanced diet while avoiding allergens.
- Medical identification: Wearing medical identification, such as a MedicAlert® bracelet, is a simple yet critical safety measure that communicates your allergies in an emergency. More information can be found at Wearing medical identification.
Frequently Asked Questions about Food Allergy Doctors
How do I find a qualified food allergy doctor?
Finding the right food allergy doctor is key to effective management. Here’s how we recommend you go about it:
- Board Certification: Always look for a physician who is board-certified in Allergy and Immunology. This ensures they have met rigorous standards of education, training, and expertise. Many allergists also hold dual certification in pediatrics or internal medicine.
- Referrals: Start with a referral from your primary care physician. They may have specific recommendations based on your needs. Word-of-mouth from trusted friends or support groups can also be valuable.
- Specialization: Consider whether you need a pediatric allergist (for children) or an adult allergist. Many practices have specialists for both.
- Reading Reviews and Hospital Affiliations: Online reviews can offer insights into patient experience, but should be considered alongside other factors. Checking for affiliations with reputable academic or medical centers can indicate a high level of expertise and access to advanced treatments. You can also use professional directories to locate qualified specialists in your area.
What's the difference between an allergist and an immunologist?
This is a common question. For practical purposes, these two specialties are almost always combined. Physicians who specialize in this field are typically referred to as "allergist-immunologists."
- An allergist primarily focuses on diagnosing and treating allergic diseases, such as food allergies, asthma, and eczema.
- An immunologist focuses on disorders of the immune system, which can range from autoimmune conditions to primary immunodeficiencies.
The American Board of Allergy and Immunology (ABAI) certifies physicians in both specialties, meaning a board-certified allergist is also a board-certified immunologist. So, when you're looking for a food allergy doctor, you're looking for an allergist-immunologist who has expertise in food-related immune responses.
Can food allergies be outgrown?
Yes, many food allergies, particularly in children, can be outgrown! This is a source of hope for many families and another reason why a long-term partnership with a food allergy doctor is so important.
- Common Allergies in Children: Allergies to milk, eggs, soy, and wheat are often outgrown during childhood. Research has explored factors that influence the likelihood of outgrowing these allergies.
- Allergies That Tend to Be Lifelong: Allergies to peanuts, tree nuts, fish, and shellfish are generally less likely to be outgrown and often persist into adulthood. However, new treatments like OIT are changing the landscape.
- Role of an Allergist in Re-testing: Your allergist will regularly monitor your child's allergies and may recommend periodic re-testing (using blood tests or an oral food challenge) to determine if an allergy has been outgrown. This allows for the safe reintroduction of foods into the diet if tolerance develops.
Conclusion
Navigating food allergies can feel daunting, but it doesn't have to be a journey of fear and limitation. The right food allergy doctor is more than just a medical professional; they are a critical partner who can transform your experience from one of constant anxiety to one of informed empowerment.
We've explored how a dedicated allergist can help you understand your unique symptoms, provide accurate diagnoses through comprehensive testing, and offer cutting-edge treatment options like Oral Immunotherapy that go beyond mere avoidance. We’ve also highlighted the vital role of your allergist in creating personalized management plans, ensuring emergency preparedness, and supporting your long-term quality of life by addressing both the physical and emotional aspects of living with food allergies.
The goal isn't just to survive with food allergies, but to thrive. By partnering with a top food allergy doctor, you gain access to the latest scientific advancements, compassionate care, and the knowledge needed to make confident decisions for yourself and your family.
At Dr. Doug Jones, we believe in redefining complex immune challenges and empowering individuals with lasting relief through personalized care and education. We're here to help you move from a life of fear to one where you feel in control, confident, and free. Take the next step in understanding your immune health and reclaiming your life.
