Integrative Immunology 101
Unlock robust immune health with integrative immunology. Learn how lifestyle, research, and personalized care transform your well-being.

Why Understanding Integrative Immunology Matters for Your Health
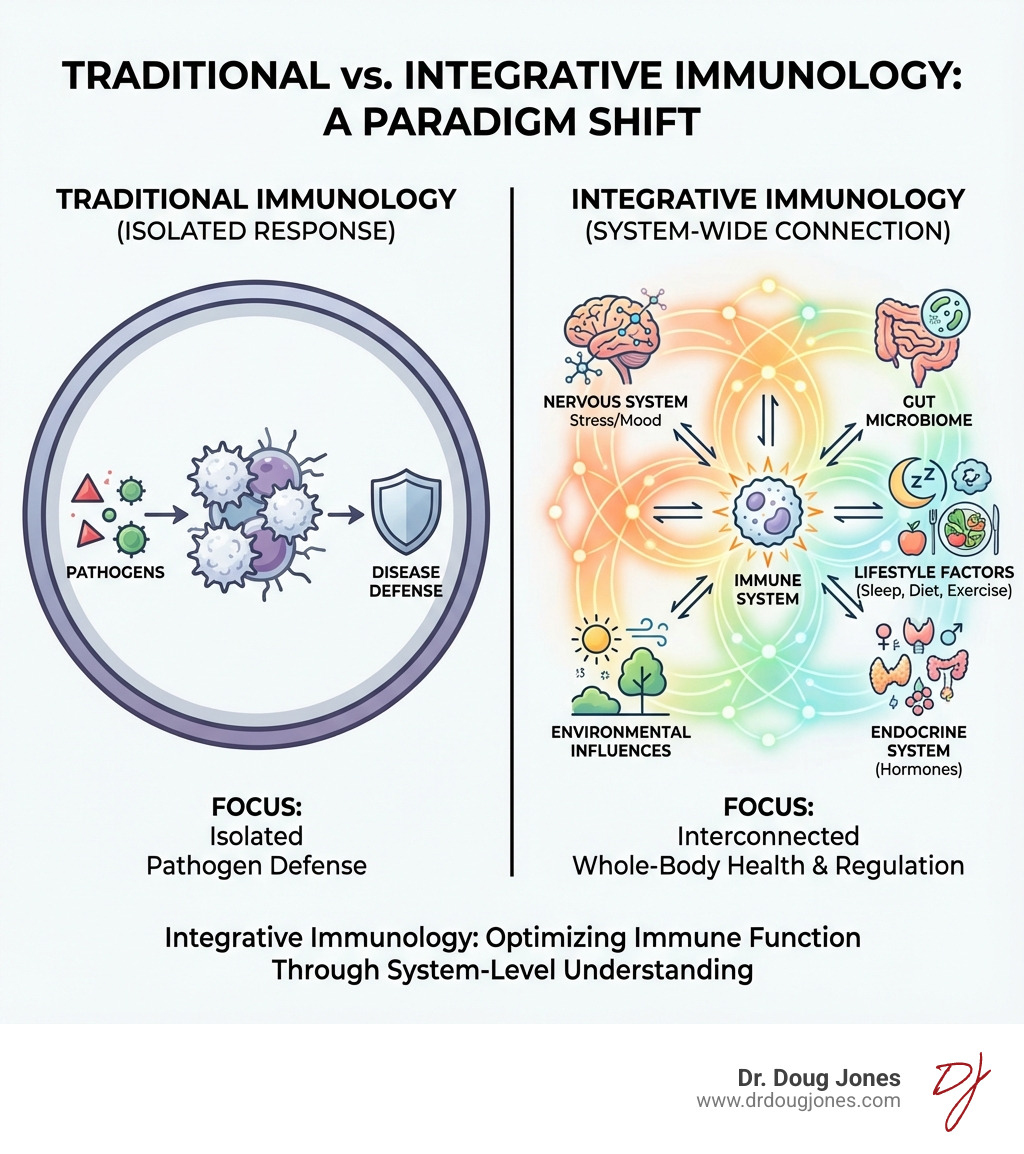
Integrative immunology is a modern approach that views the immune system not as an isolated defense force, but as a complex network deeply connected to your brain, gut, hormones, and even your environment. While traditional immunology focuses on how immune cells fight specific pathogens, integrative immunology looks at the bigger picture: how lifestyle, diet, stress, and other factors influence your overall immune health.
The goal is to move beyond just treating symptoms and instead understand and address the root causes of immune dysfunction. This is especially crucial for managing chronic conditions like allergies, autoimmune diseases, and long COVID, where the immune system's balance is key.
This approach combines cutting-edge science with practical, evidence-based lifestyle interventions. It empowers you with the knowledge and tools to support your body's natural defenses, prevent disease, and support lasting well-being.
I'm Dr. Doug Jones, a board-certified immunologist and founder of the Global Allergy Immune Network (GAIN). I apply integrative immunology principles to help patients with complex immune conditions—from food allergies and mast cell activation to long COVID and chronic fatigue—find real, sustainable solutions. Through this guide, I'll break down how this approach works, what the science says, and how you can use it to take control of your health.
The Core Principles and System-Wide Impact
At its heart, integrative immunology recognizes that the immune system is not a standalone army but a deeply interconnected part of your body's entire ecosystem. It shifts focus from isolated cells to the bigger picture, asking how the immune system interacts with the brain, gut, and hormones to influence overall health.
A key concept is chronic inflammation. Unlike acute inflammation that helps you heal, chronic, low-grade inflammation is a persistent state of alert that can contribute to many modern diseases, including heart disease, diabetes, and autoimmune conditions.
The Holistic Approach of Integrative Immunology
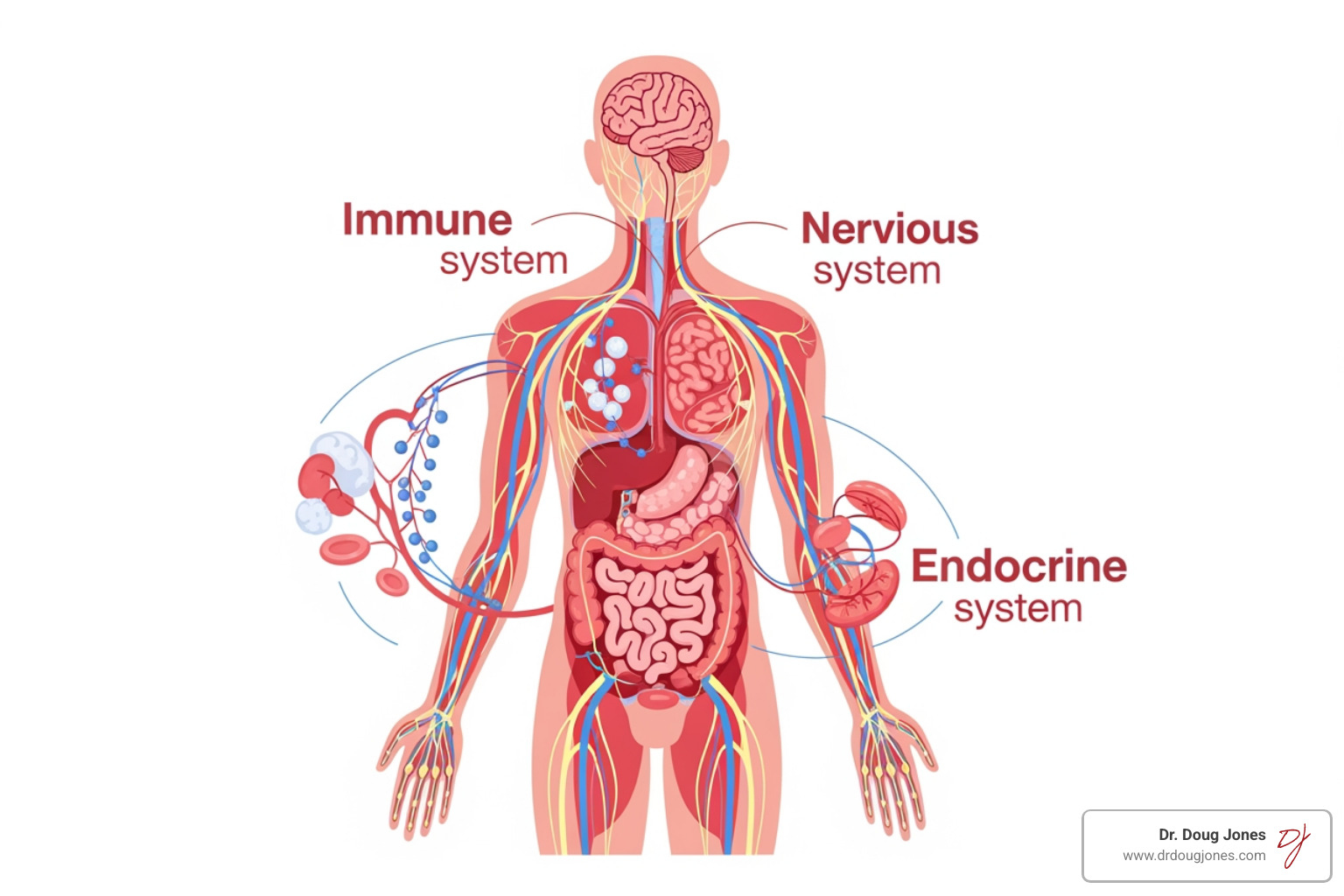
Your immune system is in constant communication with other major systems:
- The Neuro-Immune Axis: Your brain and immune system are directly linked. Stress can weaken your immune response, while inflammation can affect your mood and cognitive function.
- The Gut-Brain-Immune Connection: The trillions of microbes in your gut play a huge role in regulating immunity. An imbalanced gut microbiome is linked to allergies and autoimmune diseases.
- Endocrine System Interactions: Hormones are powerful chemical messengers that influence immune cells, affecting everything from metabolism to stress response.
The Role of Lifestyle in Shaping Your Immunity
One of the most empowering aspects of integrative immunology is that your daily choices profoundly impact your immune health:
- Nutrition: A diet rich in whole foods and healthy fats helps reduce inflammation. Key micronutrients like vitamins C, D, and zinc are essential for proper immune function.
- Exercise: Regular, moderate physical activity supports immune balance and lowers chronic illness risk.
- Sleep: Getting 7-8 hours of quality sleep is crucial. Lack of sleep increases inflammation and susceptibility to infections.
- Stress Management: Chronic stress weakens immunity. Meditation and mindfulness can reduce inflammation and improve immune responses.
- Social Connections: Strong social ties have been shown to benefit immune function.
For more on how diverse data streams are integrated to understand these complex relationships, explore the insights from Scientific research on data integration for immunology.
The Cutting Edge: Research and Methodologies
The field of integrative immunology is rapidly advancing, driven by technological breakthroughs that allow us to probe the immune system with unprecedented detail. Systems immunology integrates systems biology with immunology, using computational modeling to understand the immune system as a complex, dynamic network.
High-Tech Tools for Understanding Health
To solve the immune system's complexity, integrative immunology relies on advanced tools:
- Multi-Omics Approaches: Integrating data from genomics (genes), proteomics (proteins), and metabolomics (metabolites) to get a complete picture of health at a molecular level.
- Advanced Cytometry: Technologies like flow cytometry and CyTOF allow detailed analysis of individual immune cells, identifying their type, function, and activation state.
- Bioinformatics and AI: Powerful computers and artificial intelligence help scientists identify patterns in large datasets, predict immune responses, and design new therapies.
Future Frontiers in Research
The future of integrative immunology holds immense promise:
- Personalized Medicine: Understanding your unique genetic, environmental, and lifestyle factors allows treatments customized specifically to you.
- "Trained Immunity" and Universal Vaccines: Research explores how to "train" the immune system to respond more effectively to diverse threats.
- Advanced Modeling: Computational models are becoming increasingly sophisticated, allowing researchers to simulate immune responses and test therapies virtually.
While challenges remain in standardizing and interpreting vast amounts of data, collaborative efforts between doctors, scientists, and data analysts are paving the way for personalized and preventative healthcare. For more, see the Integrated organ immunity research.
Integrative Immunology in Action: From Lab to Life
The ultimate goal of all this cutting-edge research in integrative immunology is to translate complex scientific understanding into tangible benefits for human health. This means moving beyond the lab bench and into clinical care, offering improved health outcomes for real people.
In practice, this approach can support more effective chronic disease management and the development of personalized treatment plans. By understanding the unique interplay of an individual's genetics, lifestyle, and environment with their immune system, clinicians can better target the root contributors to health challenges, rather than just masking symptoms.
A New Paradigm for Cancer Treatment
The immune system's role in cancer is a prime example of where integrative immunology is making significant strides. We now understand that the immune system is not merely a passive bystander in cancer development; it actively influences carcinogenesis, cancer-associated morbidity, and a patient's response to therapy.
- Immuno-oncology: This rapidly evolving field harnesses the body's own immune system to fight cancer. Treatments like checkpoint blockade, which target proteins like PD-1, have changed cancer therapy by releasing the immune system's attack on tumors.
- Tumor Microenvironment: Integrative approaches emphasize understanding the complex ecosystem surrounding a tumor, which includes various immune cells, stromal cells, and signaling molecules. This microenvironment can either promote or hinder the immune response against cancer.
- Innate and Adaptive Resistance: By integrating insights into both the rapid, non-specific innate immune responses and the targeted, memory-forming adaptive responses, researchers can design combination therapies that better address cancer's evasive strategies.
For more information on the immune system's role in cancer and its treatment, the National Cancer Institute resources offer extensive information.
Tackling Aging and Chronic Inflammation
Age-related pathologies are another critical area benefiting from integrative immunology. As we discussed, the immune system changes with age, contributing to a state often referred to as "inflammaging"—a chronic, low-grade inflammation that drives many age-related diseases.
This integrated understanding is vital for tackling:
- Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and multiple sclerosis, where the immune system mistakenly attacks the body's own tissues, often involve complex genetic predispositions interacting with environmental and lifestyle triggers. An integrative approach seeks to identify and modulate these triggers. If you're struggling with symptoms of an autoimmune disease, we offer autoimmune disease help and address concerns like auto-immune disorder chronic stomach pain.
- Cardiovascular Disease: Chronic inflammation is a key driver of heart disease.
- Diabetes: Both type 1 (autoimmune) and type 2 (metabolic) diabetes have significant immune and inflammatory components.
Here's a simplified look at how lifestyle factors can influence inflammatory markers:
| Lifestyle Factor | Effect on Inflammation |
|---|---|
| Nutrition | An anti-inflammatory diet (rich in fruits, vegetables, fiber, and healthy fats) is associated with lower inflammatory markers, while a diet high in processed foods and sugar promotes inflammation. |
| Exercise | Regular, moderate exercise tends to lower systemic inflammation and is linked to reduced levels of markers such as C-reactive protein (CRP). |
| Stress | Chronic stress increases pro-inflammatory cytokines; stress management techniques like meditation and mindfulness are linked to reductions in these markers. |
| Sleep | Sleep deprivation is associated with higher levels of inflammatory markers like CRP and IL-6; consistent, quality sleep helps regulate the inflammatory response. |
Frequently Asked Questions about Integrative Immunology
What is the main goal of an integrative immunology approach?
The main goal of an integrative immunology approach is to optimize your whole-body health by understanding and supporting your immune system's intricate connections with all other bodily systems. The focus is on moving beyond merely managing symptoms to address the root contributors to immune dysfunction, whether it's an overactive response in allergies or autoimmune conditions, or an underactive one leading to frequent infections.
This involves:
- Optimizing Whole-Body Health: Recognizing that immune health is about protection, repair, healing, and maintaining overall balance.
- Preventing Disease: By understanding early signs of immune dysregulation and addressing lifestyle factors, we can work to prevent or slow the onset of chronic conditions like age-related cardiovascular and metabolic diseases, and some cancers.
- Creating Personalized Strategies: Each person's immune system is unique, influenced by genetics, environment, and lifestyle. An integrative approach allows for highly personalized treatment and wellness plans. This is where personalized allergy care is essential, as broad food allergy panels often miss the nuances of individual immune responses.
- Addressing Root Contributors: Instead of simply suppressing an immune response (for example, with steroids for asthma), we ask why the immune system is reacting the way it is. Understanding the "allergy root cause" can lead to more effective and lasting relief.
- Moving Beyond Symptom Management: While symptom relief is important, the ultimate aim is to support immune balance for lasting well-being. This is particularly relevant for complex, chronic conditions like long COVID, where addressing underlying immune dysregulation is key to finding relief.
Can lifestyle changes really make a difference to my immune system?
Absolutely. Scientific evidence shows that daily habits are powerful modulators of immune function.
- Nutrition: A balanced, anti-inflammatory diet rich in vitamins and minerals is crucial for a healthy immune response.
- Exercise: Regular, moderate activity can support immunity and reduce inflammation.
- Sleep: Getting 7-8 hours of quality sleep is essential for immune cell function and repair.
- Stress Management: Chronic stress weakens the immune system, while practices like meditation and mindfulness can have measurable benefits.
- Social Connections: Positive social relationships have been shown to have a beneficial impact on immune function.
Is integrative immunology the same as functional medicine?
While closely related and often overlapping, integrative immunology and functional medicine are not exactly the same, but they are complementary.
- Integrative Immunology as a Scientific Field: Integrative immunology is primarily a scientific and research-driven field. It studies the complex, multi-system interactions of the immune system, utilizing advanced methodologies like multi-omics, computational modeling, and AI to understand the "why" and "how" of immune function and dysfunction.
- Functional Medicine as a Clinical Model: Functional medicine is a clinical model of care. It uses the principles of systems biology and root-cause analysis to address chronic disease. Functional medicine practitioners draw on insights from integrative immunology to guide their clinical practice, focusing on patient-centered care and lifestyle interventions.
Both approaches share a commitment to seeking out and addressing the underlying drivers of illness, rather than just treating symptoms. Integrative immunology generates much of the scientific knowledge about how the immune system interacts with nutrition, stress, the microbiome, genetics, and environment, while functional medicine applies that knowledge in the clinic.
The Cutting Edge: Research and Methodologies
The field of integrative immunology is rapidly advancing, driven by technological breakthroughs that allow us to probe the immune system with unprecedented detail. This is where systems immunology, multi-omics, and computational power come into play, helping us piece together the incredibly complex puzzle of immune health.
Systems immunology integrates systems biology with immunology, using computational and mathematical modeling to understand the immune system as a complex, dynamic, and multiscale network. The immune system, with its vast number of cells and signaling molecules, is one of the most intricate systems in the body, making a systems approach indispensable.
At the Laboratory of Integrative Cancer Immunology (LICI) at the National Cancer Institute, for example, researchers use interdisciplinary approaches that combine biological, molecular, and computational methods, bioinformatics, genetics, mathematical modeling, and transkingdom network analysis. This allows them to study the immune system's role in carcinogenesis, cancer-associated morbidity, and response to cancer therapy, with a focus on interactions between innate and adaptive resistance.
This approach acknowledges that immune-mediated diseases often stem from the dysregulation of multiple targets and pathways, moving beyond traditional single-target drug development.
High-Tech Tools for Understanding Health
To address the immune system's complexity, integrative immunology relies on a suite of advanced tools and methodologies:
Multi-Omics Approaches: Integrating data from various "omics" fields to get a holistic view:
- Genomics: Studying our entire genetic makeup, including genetic variations (single nucleotide polymorphisms or SNPs) and the highly polymorphic human leukocyte antigen (HLA) region, which are crucial for immune responses and disease susceptibility.
- Epigenetics: Examining changes in gene expression that do not alter the DNA sequence, such as DNA methylation and histone modifications. These can be influenced by environmental factors and lifestyle.
- Transcriptomics: Analyzing all the RNA molecules (transcripts) in a cell or organism, revealing which genes are active and how their activity changes in different conditions.
- Proteomics: Studying the entire set of proteins produced or modified by an organism, providing insights into cellular function and pathways.
- Metabolomics: Analyzing small-molecule metabolites in a biological sample, reflecting the current physiological state and metabolic processes.
Cytometry (Flow Cytometry & CyTOF): These techniques allow for detailed analysis of individual immune cells, identifying different cell types, their activation states, and expression of various markers. Mass cytometry (CyTOF) uses metal isotopes instead of fluorophores, allowing simultaneous measurement of many parameters per cell.
Bioinformatics and Computational Modeling: Essential for making sense of massive datasets generated by omics technologies.
- Computational Modeling: Creating mathematical models to simulate immune responses and predict outcomes.
- Bioinformatics: Using computational tools to analyze biological data, identify patterns, and draw conclusions, including analysis of immune repertoires (TCR and BCR sequencing).
- Transkingdom Network Analysis: Examining interactions across different biological kingdoms, such as between human host cells and microbial communities (for example, the gut microbiome), to better understand host-microbiome interactions.
Data Repositories: Global repositories store and share information, facilitating large-scale analyses and collaborations. Examples include dbGaP, GWAS Catalog, GEO, ENCODE, SRA, ImmPort, PIRD, the Human Microbiome Project, and others.
Artificial Intelligence (AI) in Immunology: AI, including machine learning and deep learning, is rapidly becoming a cornerstone of integrative immunology. It helps:
- Identify novel immune pathways and interactions.
- Predict biomarkers for diagnosis, prognosis, and treatment response.
- Support personalized medicine by anticipating individual responses to therapies.
Future Frontiers in Integrative Immunology Research
The future of integrative immunology holds immense promise for changing human health. We are moving towards:
Personalized Medicine: By integrating an individual's unique genetic, environmental, and lifestyle data, we can develop more personalized treatment and prevention strategies, moving away from a "one-size-fits-all" approach.
"Trained Immunity" and Universal Vaccines: Emerging research into "trained immunity" suggests that innate immune cells can develop a form of memory, offering broader protection against various pathogens. This, along with "integrated organ immunity" (where innate and adaptive systems interact with non-haematopoietic cells in tissues), may support the development of vaccines that protect against diverse pathogens, as explored in recent Integrated organ immunity research.
Advanced Modeling and AI: Further advancements in computational modeling and AI will allow simulation of complex immune scenarios, prediction of disease progression, and identification of therapeutic targets with greater accuracy.
Challenges remain, including ensuring data quality and standardization across diverse datasets, validating complex models, and addressing computational demands. These challenges also present opportunities for interdisciplinary collaboration—bringing together clinicians, immunologists, bioinformaticians, statisticians, and AI specialists, and training the next generation with these integrated skills.
Integrative Immunology in Action: From Lab to Life
The ultimate goal of integrative immunology research is translating complex scientific understanding into tangible health benefits. This means moving beyond the lab bench into clinical care, offering improved outcomes for real people.
In practice, this approach supports more effective chronic disease management and personalized treatment plans. By understanding the unique interplay of genetics, lifestyle, and environment with the immune system, we can tailor interventions that address root contributors to health challenges.
A New Paradigm for Cancer Treatment
The immune system's role in cancer exemplifies where integrative immunology is making significant strides. We now understand that the immune system actively influences carcinogenesis and treatment response:
- Immuno-oncology: This field harnesses the body's immune system to fight cancer. Treatments like checkpoint blockade have revolutionized cancer therapy.
- Tumor Microenvironment: Understanding the complex ecosystem surrounding tumors helps determine whether the immune response promotes or hinders cancer treatment.
- Innate and Adaptive Resistance: Integrating insights into both rapid innate and targeted adaptive responses enables more effective combination therapies.
For more information, the National Cancer Institute resources offer extensive information.
Tackling Aging and Chronic Inflammation
Age-related pathologies benefit from integrative immunology. "Inflammaging"—chronic, low-grade inflammation—drives many age-related diseases. This understanding is vital for tackling:
- Autoimmune Diseases: Conditions like rheumatoid arthritis and lupus involve complex genetic predispositions interacting with environmental triggers. If you're struggling with autoimmune symptoms, we offer autoimmune disease help and address concerns like auto-immune disorder chronic stomach pain.
- Cardiovascular Disease: Chronic inflammation is a key driver of heart disease.
- Diabetes: Both type 1 and type 2 diabetes have significant immune and inflammatory components.
| Lifestyle Factor | Effect on Inflammation |
|---|---|
| Nutrition | Anti-inflammatory diet (fruits, vegetables, fiber, healthy fats) lowers inflammatory markers; processed foods and sugar promote inflammation. |
| Exercise | Regular, moderate exercise lowers systemic inflammation and reduces markers like C-reactive protein (CRP). |
| Stress | Chronic stress increases pro-inflammatory cytokines; stress management techniques reduce these markers. |
| Sleep | Sleep deprivation increases inflammatory markers; consistent, quality sleep helps regulate inflammatory response. |
Frequently Asked Questions about Integrative Immunology
What is the main goal of an integrative immunology approach?
The main goal is optimizing whole-body health by understanding and supporting your immune system's intricate connections with all other bodily systems. The focus moves beyond managing symptoms to address root contributors to immune dysfunction.
This involves:
- Optimizing Whole-Body Health: Recognizing that immune health encompasses protection, repair, healing, and maintaining overall balance.
- Preventing Disease: Understanding early signs of immune dysregulation and addressing lifestyle factors to prevent chronic conditions.
- Creating Personalized Strategies: Each person's immune system is unique. An integrative approach allows for highly personalized treatment plans.
- Addressing Root Contributors: Instead of simply suppressing immune responses, we ask why the immune system is reacting as it is.
- Moving Beyond Symptom Management: While symptom relief is important, the ultimate aim is supporting immune balance for lasting well-being.
Can lifestyle changes really make a difference to my immune system?
Yes. The impact of lifestyle on the immune system is one of the most important insights from integrative immunology:
- Nutrition: Micronutrients like vitamins C, D, and zinc are critical for immune function. An anti-inflammatory diet rich in fiber and omega-3 fats helps counter chronic inflammation.
- Exercise: Moderate, regular exercise supports immune function and has measurable anti-inflammatory effects.
- Sleep: Adequate sleep (7-8 hours) strengthens immune responses. Sleep deprivation increases inflammatory markers.
- Stress and Mindfulness: Chronic stress suppresses immune function. Mindfulness meditation has been associated with decreased inflammatory markers.
These are evidence-based levers you can use to positively influence your immune health.
Is integrative immunology the same as functional medicine?
While closely related, they are complementary but not identical:
- Integrative Immunology as a Scientific Field: It's primarily research-driven, studying complex immune system interactions using advanced methodologies like multi-omics and AI.
- Functional Medicine as a Clinical Model: It's a clinical care model using systems biology principles and root-cause analysis to address chronic disease.
Both share a commitment to addressing underlying drivers of illness rather than just treating symptoms. Integrative immunology generates scientific knowledge about immune system interactions, while functional medicine applies that knowledge in clinical practice.
Conclusion: Taking an Integrative Approach to Your Immune Health
We have explored the complex and fascinating world of integrative immunology, looking at how the immune system is intertwined with every aspect of our biology—from our genes and gut microbes to our daily habits and emotional states. This holistic perspective offers powerful ways to understand and address health challenges, moving beyond traditional, fragmented views of disease.
The benefits of embracing an integrative approach are clear: greater understanding of your own body, opportunities for prevention, and the potential for more durable relief from complex immune challenges. By understanding the core principles, leveraging cutting-edge research, and implementing evidence-based lifestyle interventions, you can actively support a more robust and balanced immune system.
This is the philosophy that guides our work at Dr. Doug Jones. We focus on understanding your unique immune story and providing personalized care and education to address the root contributors to your symptoms. Whether you're navigating food allergies, struggling with long COVID, or seeking to optimize your overall immune health, an integrative approach offers a thoughtful, science-informed path forward.
Ready to take the next step with your immune health?
Find personalized immune health solutions
