Chronic Fatigue Syndrome: What You Need to Know About ME/CFS
Understand chronic fatigue syndrome: symptoms, causes, diagnosis, and management strategies for this debilitating illness. Learn how to live better.

Understanding a Serious and Complex Chronic Illness
Chronic fatigue syndrome (also called Myalgic Encephalomyelitis, or ME/CFS) is a serious, long-term illness that affects many body systems and keeps people from doing their usual activities. Here's what you need to know:
Quick Facts About ME/CFS:
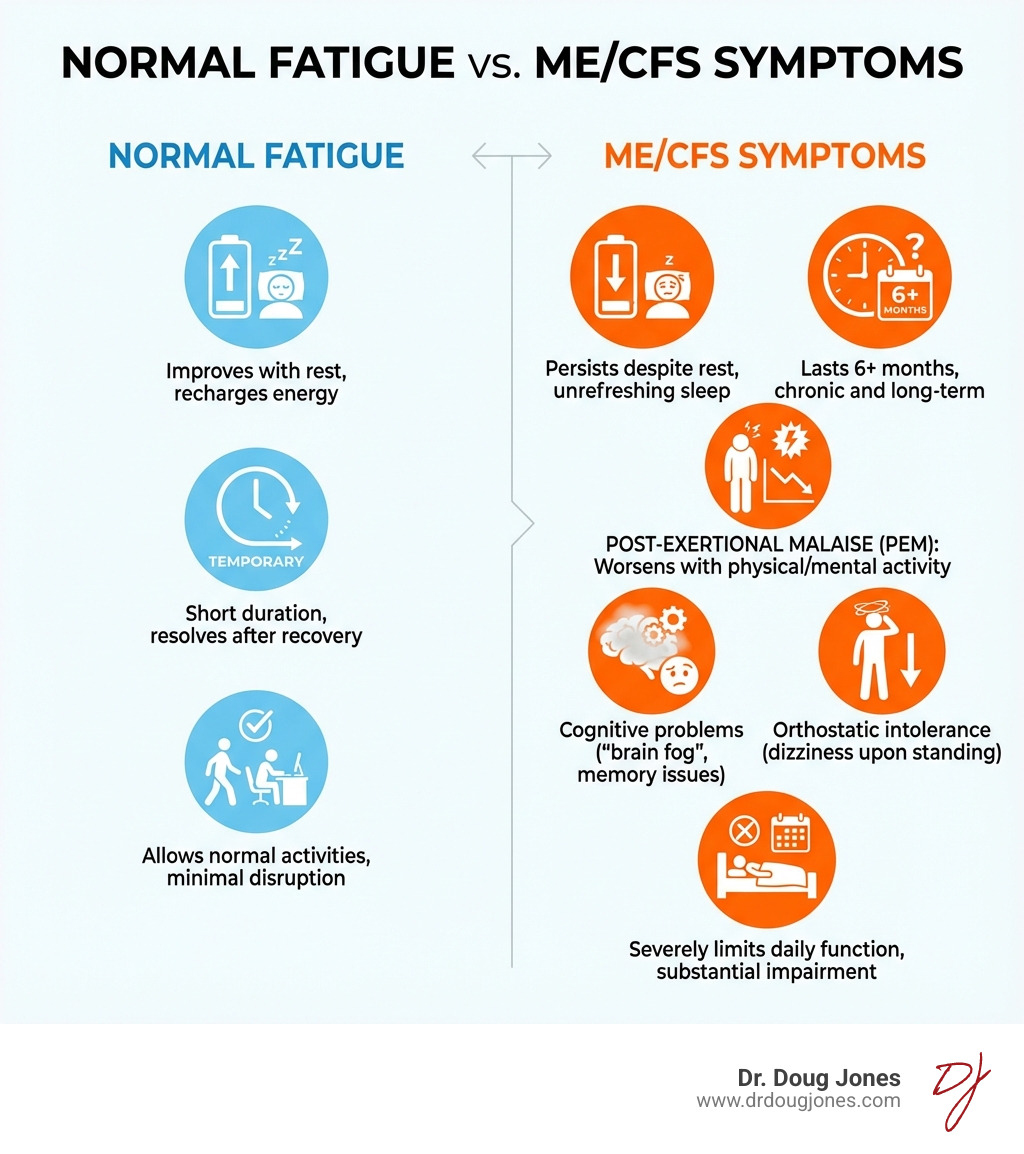
- Not just tiredness - It's severe fatigue that doesn't improve with rest and worsens with physical or mental activity
- Core symptoms - Extreme exhaustion after activity (post-exertional malaise), unrefreshing sleep, and problems with thinking/memory
- Affects millions - Up to 3.3 million people in the United States have ME/CFS
- Mostly undiagnosed - More than 9 in 10 people with ME/CFS have not been diagnosed by a doctor
- Serious impact - About 1 in 4 people with ME/CFS are confined to bed at some point
- No cure yet - Treatment focuses on managing symptoms and improving quality of life
ME/CFS is not a psychological disorder. It's a biological illness that causes real, measurable changes in your immune system, nervous system, and energy metabolism. While the exact cause remains unknown, many cases start after an infection - between 60% and 80% of cases begin after a viral illness.
The hallmark symptom is post-exertional malaise (PEM) - a worsening of symptoms after even minor physical or mental effort. This can last for days, weeks, or longer. Simple activities like grocery shopping, taking a shower, or having a conversation can trigger a "crash."
ME/CFS often strikes people in their most productive years, with the condition most common between ages 40 and 60. Women are diagnosed two to four times more often than men. Some people become so severely affected that they cannot work, attend school, or maintain basic self-care.
As an immunologist specializing in complex chronic conditions, I've worked with many patients struggling with chronic fatigue syndrome and related immune challenges, helping them find personalized approaches to manage symptoms and improve their quality of life. My practice focuses on understanding the underlying immune dysfunction that drives ME/CFS and developing targeted strategies for each individual.
The Debilitating Symptoms of ME/CFS
When we talk about chronic fatigue syndrome, we're not just discussing feeling a bit tired after a long day. We're talking about a profound, pervasive exhaustion that fundamentally alters a person's life. The symptoms of ME/CFS are far-reaching and can fluctuate dramatically, making it an unpredictable and challenging condition to live with.
The severity of ME/CFS can vary greatly from person to person. Roughly one-quarter of those living with ME/CFS fall into the mild category, where they can still perform some daily activities but with significant effort and limitations. Half fall into the moderate or moderate-to-severe categories, experiencing substantial reductions in activity and often needing to modify their lives significantly. A smaller, but still significant, portion experiences severe or very severe ME/CFS, which can render them homebound or even bed-bound. In fact, about 1 in 4 people with ME/CFS are confined to bed at some point in their illness.
The Core Symptoms of Chronic Fatigue Syndrome
The diagnosis of ME/CFS hinges on a set of core symptoms that distinguish it from other fatigue-related conditions. According to the Institute of Medicine (IOM) 2015 diagnostic criteria, which many healthcare providers now follow, these are the essential pillars of the illness:
- Substantial Reduction in Activity (with Profound Fatigue): Before the illness, individuals could engage in certain activities, but now they experience a significant and persistent decline in their ability to perform these activities. This isn't just being tired; it's a deep-seated exhaustion that doesn't go away with rest.
- Post-Exertional Malaise (PEM) Crash: This is arguably the most characteristic and debilitating symptom of ME/CFS. PEM is the worsening of symptoms after even minor physical, mental, or emotional exertion. The "crash" can be delayed, often appearing 12 to 48 hours after the activity, and can last for days, weeks, or even months. Imagine feeling okay enough to do some light chores, only to be completely wiped out and bedridden for days afterward. This unpredictable "push-crash" cycle makes planning and maintaining any semblance of a normal life incredibly difficult.
- Unrefreshing Sleep: Despite spending adequate time in bed, individuals with ME/CFS do not feel rested or refreshed upon waking. Sleep may be fragmented, light, or characterized by unusual patterns, leaving them feeling as exhausted as when they went to bed.
- Problems with Thinking and Memory (Cognitive Impairment): Often referred to as "brain fog," this symptom includes difficulties with memory, concentration, information processing, and finding the right words. It can make everyday tasks like following conversations, reading, or working on a computer feel overwhelming and inefficient.
- Worsening Symptoms While Standing or Sitting Upright (Orthostatic Intolerance): Many people with ME/CFS experience symptoms like lightheadedness, dizziness, blurred vision, heart palpitations, or increased fatigue when they stand or sit upright for extended periods. This often improves when lying down. Common forms include Postural Orthostatic Tachycardia Syndrome (POTS) and Neurally Mediated Hypotension (NMH).
These core symptoms must be present for at least six months and significantly impact a person's life to warrant an ME/CFS diagnosis. You can learn more about these symptoms on the CDC's dedicated page: Symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.
Other Common Symptoms
Beyond the core diagnostic criteria, individuals with chronic fatigue syndrome often experience a range of other distressing symptoms that contribute to their overall suffering. These associated symptoms highlight the multi-systemic nature of ME/CFS:
- Widespread Pain: This can manifest as muscle pain (myalgia), joint pain (arthralgia) without swelling or redness, and persistent headaches, including migraines. The pain can be severe and migratory, making daily activities even more challenging.
- Sore Throat and Tender Lymph Nodes: Frequent sore throats and tender, often swollen, lymph nodes in the neck or armpits are common.
- Chills and Night Sweats: Many patients report experiencing unexplained chills or drenching night sweats, suggesting a dysregulation in body temperature control.
- Sensitivities: An increased sensitivity to various environmental factors is often reported. This can include:
- Light (Photophobia): Bright lights can be painful or overwhelming.
- Sound (Hyperacusis): Normal sounds can seem excessively loud or irritating.
- Smells: Strong odors, including perfumes or chemicals, can trigger symptoms.
- Food and Medicines: Some individuals develop new allergies or intolerances to certain foods or medications.
- Digestive Issues: Symptoms similar to Irritable Bowel Syndrome (IBS) are frequently reported, including abdominal pain, bloating, constipation, or diarrhea. This can significantly impact diet and nutrition. (For more on related conditions, see our article on Autoimmune Disorder & Chronic Stomach Pain.)

These additional symptoms, combined with the core criteria, paint a picture of a complex illness that affects almost every aspect of a person's physical and mental well-being. It's a tough hand to be dealt, and understanding the full spectrum of symptoms is the first step toward effective management.
Understanding the Causes and Diagnosis of Chronic Fatigue Syndrome
One of the most frustrating aspects of chronic fatigue syndrome for both patients and healthcare providers is the elusive nature of its cause. Despite extensive research, there isn't one single, definitive cause that applies to everyone. Instead, it's believed to be a complex interplay of various factors that can trigger and perpetuate the illness. Furthermore, the absence of a specific diagnostic test means that diagnosis often involves a thorough process of elimination.
Potential Causes and Risk Factors
While the exact cause remains unknown, several theories and risk factors have emerged from scientific study:
Infection Trigger: A significant number of ME/CFS cases, between 60% and 80%, start after an infection, most often viral. Common culprits include:
- Epstein-Barr Virus (EBV): The virus that causes infectious mononucleosis (mono). Around 15% to 50% of people who get infectious mononucleosis develop ME/CFS.
- SARS-CoV-2 (COVID-19): We've seen a clear link between COVID-19 infection and the development of ME/CFS-like symptoms, often referred to as Long COVID. Many individuals with Long COVID meet the diagnostic criteria for ME/CFS. This connection has brought renewed attention and research interest to post-viral syndromes. You can explore more about post-viral syndromes in Scientific research on post-viral syndromes and learn about Long COVID Symptoms: You're Not Alone & You're Not Imagining It.
- Other infections like Ross River virus and Q fever have also been implicated. The idea is that an acute infection might "hit and run," leaving behind lasting immune or neurological dysregulation.
Immune System Changes: Research suggests that the immune system in people with ME/CFS doesn't function quite right. This can include:
- Impaired function of natural killer (NK) cells and T cells, which are crucial for fighting infections.
- Abnormal cytokine production, leading to chronic inflammation.
- Presence of autoantibodies, suggesting an autoimmune component where the body mistakenly attacks its own tissues.
Cellular Energy Production Issues: Some studies point to problems with how cells convert fats and sugars into energy, particularly within the mitochondria, the "powerhouses" of our cells. This could explain the profound fatigue and post-exertional malaise.
Genetic Predisposition: ME/CFS appears to run in some families, suggesting that genetic factors may increase an individual's susceptibility. This doesn't mean you'll definitely get it if a family member has it, but it might mean you're more prone if other triggers are present.
Physical or Emotional Trauma: Significant physical trauma (like surgery or injury) or severe emotional stress can sometimes precede the onset of ME/CFS, acting as a trigger in vulnerable individuals.
Gender: ME/CFS affects women much more often than men, typically two to four times more frequently. This gender disparity is a subject of ongoing research, possibly linking to hormonal differences or how immune systems respond.
Age: While anyone can develop ME/CFS, it's most commonly diagnosed in young to middle-aged adults, with a peak incidence between 40 and 60 years old.
How Doctors Diagnose ME/CFS
Diagnosing chronic fatigue syndrome is a bit like being a detective. There's no single blood test or scan that definitively says, "Aha! You have ME/CFS!" Instead, doctors must carefully review symptoms, medical history, and conduct various tests to rule out other conditions that could cause similar symptoms. This process can be lengthy and frustrating for patients, leading to significant diagnostic delays.
The CDC provides valuable guidance on the diagnostic process: Diagnosing ME/CFS.
Here's how we typically approach the diagnosis:
- Comprehensive Medical History and Physical Exam: This is where we gather crucial information about your symptoms, their duration, severity, and how they impact your daily life. We'll ask about your health history, family history, and any potential triggers.
- Symptom Criteria: The IOM 2015 diagnostic criteria are widely used. For a diagnosis, the patient must have:
- A substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities that persists for more than 6 months and is accompanied by fatigue that is often profound.
- Post-exertional malaise (PEM).
- Unrefreshing sleep.
- At least one of the following: cognitive impairment OR orthostatic intolerance.These symptoms must be present at least half the time with moderate or severe intensity.
- Ruling Out Other Conditions: This is a critical step, as many other illnesses can mimic ME/CFS. We'll often use various laboratory tests to exclude these possibilities. Here's a list of conditions we typically consider:
- Sleep Disorders: Such as sleep apnea, restless legs syndrome, or narcolepsy.
- Thyroid Issues: Hypothyroidism can cause fatigue, weight gain, and cognitive problems.
- Anemia: Low red blood cell count can lead to fatigue.
- Autoimmune Diseases: Conditions like lupus, rheumatoid arthritis, or Sjögren's syndrome.
- Infections: Persistent or chronic infections that could be causing fatigue.
- Neurological Disorders: Multiple sclerosis (MS) or other conditions affecting the nervous system.
- Mental Health Conditions: While ME/CFS is not a psychological disorder, depression, anxiety, or other mood disorders can cause fatigue and need to be evaluated separately.
- Nutritional Deficiencies: Such as Vitamin D or B12 deficiency.
- Medication Side Effects: Certain drugs can cause fatigue.
- Cancer: Though rare, serious illnesses must always be considered.
This process can be frustrating, and many patients feel unheard or dismissed during their diagnostic journey. If you're struggling to get answers, remember our tips for navigating the healthcare system: 8 Tips for When You Don't Feel Heard by Your Doctor and From Specialist to Specialist: Why You Still Don't Have Answers & What to Do Next.
Managing and Living with ME/CFS
Living with chronic fatigue syndrome is a daily challenge, characterized by unpredictability and significant limitations. While there is currently no cure, the focus of treatment is firmly on managing symptoms, improving quality of life, and preventing potential complications. This often requires a multidisciplinary team approach, involving physicians, physical therapists, occupational therapists, and mental health professionals.
Managing Life with Chronic Fatigue Syndrome
The cornerstone of managing ME/CFS is learning to live within your body's new limits. This is where strategies like "pacing" and understanding your "energy envelope" become vital. The CDC offers excellent resources on managing the condition: Manage Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.
- Pacing (Energy Management): This isn't about pushing through the fatigue; it's about carefully balancing activity and rest to avoid triggering post-exertional malaise (PEM). Pacing means breaking down tasks into smaller steps, taking frequent breaks, and not overdoing it on "good" days. It requires a deep understanding of your personal energy limits.
- Staying Within the "Energy Envelope": Each person with ME/CFS has a unique, often fluctuating, capacity for physical and mental activity. This is their "energy envelope." Exceeding this envelope almost inevitably leads to a PEM crash. Learning to identify and respect these boundaries is crucial. This might mean saying no to social engagements, delegating chores, or modifying work responsibilities.
- Activity and Rest Balance: It's a delicate dance. Too much activity leads to a crash, but too little can lead to deconditioning and other issues. The goal is to find a sustainable rhythm that maximizes function without exacerbating symptoms.
- Avoiding Push-Crash Cycles: This is the practical application of pacing. When you feel a bit better, the temptation to "catch up" on neglected tasks or activities is strong. However, for ME/CFS patients, this almost always backfires, leading to a severe worsening of symptoms. Learning to resist this urge is a significant part of living with the condition.
- Symptom Journal: Keeping a detailed log of your activities, symptoms, and energy levels can help you identify patterns, understand your triggers, and refine your pacing strategies. It's a powerful tool for self-management.
Treatment Approaches for Key Symptoms
Since there's no single cure for chronic fatigue syndrome, treatment is highly individualized and focuses on alleviating the most bothersome symptoms.
- Managing PEM: The primary strategy is pacing. There are no medications specifically approved for PEM, but careful activity management is key.
- Improving Sleep Quality: Addressing unrefreshing sleep is crucial. This might involve:
- Good Sleep Hygiene: Establishing a regular sleep schedule, creating a dark and quiet sleep environment, and avoiding screens before bed.
- Medications: Low-dose antidepressants or sleep aids might be prescribed to help with sleep architecture, though these must be used cautiously due to potential side effects and medication sensitivities common in ME/CFS.
- Pain Relief Strategies: For muscle and joint pain or headaches:
- Over-the-Counter Painkillers: NSAIDs like ibuprofen or acetaminophen may offer some relief.
- Prescription Medications: In some cases, stronger pain relievers, muscle relaxants, or neuropathic pain medications (like gabapentin or pregabalin) might be considered.
- Complementary Therapies: Gentle massage, acupuncture, heat/cold therapy, or mindfulness techniques may help some individuals.
- Medications for Orthostatic Intolerance: If orthostatic intolerance is a significant issue, medications that help regulate blood pressure and heart rate, such as fludrocortisone or midodrine, might be prescribed. Increasing fluid and salt intake can also be beneficial.
- Dietary and Nutritional Support: While no specific diet cures ME/CFS, a balanced, anti-inflammatory diet rich in whole foods can support overall health. Some individuals find relief by identifying and avoiding food sensitivities. Nutritional supplements (e.g., certain vitamins, minerals, or coenzymes) might be recommended by a healthcare provider, but always consult with a professional before starting any new supplement regimen.
- Avoiding Graded Exercise Therapy (GET): Historically, graded exercise therapy (GET) and certain forms of Cognitive Behavioral Therapy (CBT) were recommended. However, current guidelines, such as those from NICE (National Institute for Health and Care Excellence) in the UK, strongly advise against GET, as it often exacerbates PEM and can be harmful. While CBT can be useful for coping with chronic illness, it's generally not considered a cure for ME/CFS itself.
Potential Complications of ME/CFS
Living with a severe, chronic, and often misunderstood illness like ME/CFS can lead to several significant complications:
- Social Isolation: The inability to participate in social activities, work, or school often leads to profound loneliness and isolation.
- Depression and Anxiety: The chronic nature of the illness, the constant pain, the loss of independence, and the lack of understanding from others can understandably contribute to depression and anxiety. It's crucial to remember that ME/CFS is not caused by these mental health conditions, but they can be severe complications that require appropriate support and treatment.
- Reduced Quality of Life: The pervasive symptoms and functional limitations significantly diminish a person's overall quality of life.
- Disability: Many individuals with ME/CFS become severely disabled. Fewer than half of people with ME/CFS are employed, and roughly one in five have a full-time job. This has substantial personal and economic impacts.
- Medication Side Effects: Managing multiple symptoms often requires various medications, each with its own potential side effects.
Special Considerations for Children and Teens
ME/CFS can also affect children and teenagers, presenting unique challenges for patients, families, and educational systems. While it's uncommon before age 10, it more often begins in adolescence and young adulthood.
- Impact on School and Social Life: ME/CFS can severely disrupt a child's education and social development. They may struggle to attend school, complete homework, or participate in extracurricular activities. This can lead to academic setbacks, social isolation, and feelings of frustration or misunderstanding. Parents and teachers may initially mistake symptoms for school phobia.
- Different Symptom Presentation: Children might not articulate their symptoms in the same way adults do. They might complain of "feeling unwell," "not having energy," or "brain fog" that manifests as difficulty concentrating in class.
- Need for Educational Accommodations: Schools must be flexible and provide accommodations, such as reduced timetables, home-based learning, extra time for assignments, or rest periods, to help children with ME/CFS continue their education. The CDC offers specific information for families: ME/CFS in Children: Information for Families.
- Family Support: The entire family is affected. Parents often become primary caregivers, advocating for their child's health and educational needs. They may need to help monitor and manage activity levels to ensure their children can still spend quality time with family and friends.
- Prognosis: Encouragingly, children and teenagers generally have a better chance of full or partial recovery from ME/CFS than adults, although it can still be a long and challenging journey.
Conclusion: Finding a Path Forward with ME/CFS
Chronic fatigue syndrome (ME/CFS) is a complex, biological illness that profoundly impacts millions of lives. It's far more than just "feeling tired"; it's a multi-systemic disorder characterized by debilitating post-exertional malaise, unrefreshing sleep, cognitive impairment, and a host of other challenging symptoms. We've learned that it's not a psychological condition, but a genuine illness with measurable physiological changes, often triggered by infections.
The journey to diagnosis can be long and arduous, marked by the absence of a definitive test and the need to rule out many other conditions. However, the importance of a correct diagnosis cannot be overstated. It validates the patient's experience, opens the door to appropriate symptom management, and helps prevent harmful interventions.
While a cure remains elusive, there is significant hope in ongoing research. The recent focus on post-viral syndromes, particularly in the wake of Long COVID, has injected new energy and funding into understanding conditions like ME/CFS. Scientists are actively investigating potential biomarkers, genetic factors, immune dysregulation, and novel therapeutic targets.
Empowerment comes through understanding the illness, implementing personalized management strategies like pacing, and building a supportive healthcare team. Living with ME/CFS requires immense resilience, adaptability, and a commitment to listening to your body.
At Dr. Doug Jones, we believe in a new approach to complex immune challenges, including chronic fatigue syndrome. Our integrative immunology practice focuses on understanding the unique underlying immune dysfunction in each individual, moving beyond generalized treatments to personalized care. We aim to empower you with lasting relief through education and targeted strategies.
If you or a loved one are struggling with the complexities of ME/CFS or other chronic immune conditions, we invite you to explore how our specialized approach can help. We are here to listen, investigate, and help you find a path forward.
Learn more about our approach to complex immune challenges


