Decoding Adult Food Allergies: Symptoms, Causes, and Coping
Sudden adult food allergies? Understand symptoms, causes, and effective coping strategies. Take control of your health now.

Why Adult Food Allergies Are More Common Than You Think

Adult food allergies affect approximately 11% of U.S. adults—that's more than 26 million people. If you're suddenly reacting to foods you've eaten your whole life, you're not alone. Here's what you need to know:
Quick Facts About Adult Food Allergies:
- Nearly half of adults with food allergies developed them in adulthood, not childhood
- Shellfish is the #1 trigger for adult-onset allergies, followed by tree nuts and fish
- Women are more likely than men to develop adult food allergies
- The average age of first reaction is 31 years old, but allergies can develop at any age
- 81% of adults with food allergies require an epinephrine prescription, yet fewer than 1 in 4 currently have one
- Unlike childhood allergies, adult-onset food allergies typically last a lifetime
You might experience hives after eating shrimp or notice your throat tightening when you eat tree nuts. These aren't random occurrences—they're signs your immune system has fundamentally changed.
This isn't about being "picky." Adult food allergies are real, potentially life-threatening, and rising dramatically. Insurance claims for anaphylactic reactions to food jumped 377% from 2007 to 2016, with more than a third occurring in adults.
The challenge is that most resources focus on childhood allergies, leaving adults to steer confusing symptoms, delayed diagnoses, and the emotional weight of suddenly avoiding once-safe foods. This can lead to feeling isolated, anxious, or frustrated.
This guide will help you understand why adult-onset allergies develop, get an accurate diagnosis, and take control. You'll learn to differentiate allergies from intolerances, recognize dangerous symptoms, understand treatment options, and manage the emotional and social challenges.
I'm Dr. Doug Jones, a board-certified immunologist specializing in adult food allergies and other complex immune conditions at my practice, GAIN—Global Allergy Immune Network. For over a decade, I've helped thousands of patients steer the sudden onset of food allergies. My approach focuses on accurate diagnosis and personalized treatment to empower you to reclaim confidence in your daily life—whether dining out safely, traveling without fear, or understanding what's happening in your immune system.
The Unseen Epidemic: Understanding Adult Food Allergies
While food allergies are often associated with children, a growing number of adults are developing new reactions to foods they once enjoyed. This phenomenon is known as adult-onset food allergy, and it's more common than many realize.
An adult-onset food allergy is an immune-mediated reaction to a food that develops after age 18, distinct from a childhood allergy that persists. The prevalence is substantial: approximately 11% of U.S. adults (over 26 million people) have a food allergy. Strikingly, nearly half of them developed at least one allergy during adulthood, a trend some experts call an "untold epidemic."
Studies like one in the JAMA Network Open on prevalence are shedding light on the issue, indicating that at least 15% of initial food allergy diagnoses in adults are adult-onset cases.
How Adult Food Allergies Differ from Childhood Allergies
While the underlying immune mechanisms are similar, key differences between adult-onset and childhood food allergies impact diagnosis, management, and prognosis.
One of the most significant distinctions is persistence. Many childhood allergies, particularly to milk, egg, soy, and wheat, are often outgrown as the immune system matures. In contrast, adult-onset food allergies typically last a lifetime and are far less likely to resolve.
The common culprits also tend to differ. In children, milk, eggs, and peanuts are top allergens. For adults, the landscape shifts, with shellfish and tree nuts often topping the list for newly acquired allergies.
Furthermore, there's a notable gender difference. While pediatric food allergies sometimes show a male dominance, women are more likely to develop food allergies in adulthood than men. Studies have observed a female dominance, with 64% of adult-onset cases occurring in women. The mean age for a first reaction is around 31 years, but new allergies can emerge at any point between 18 and 86 years old.
The Most Common Triggers for Adult-Onset Food Allergies
While over 160 foods can cause allergic reactions, a core group accounts for most serious incidents. The "top 9" major food allergens in the U.S. are milk, eggs, fish, peanuts, sesame, shellfish, soy, tree nuts, and wheat. For adult food allergies, some stand out as new triggers.
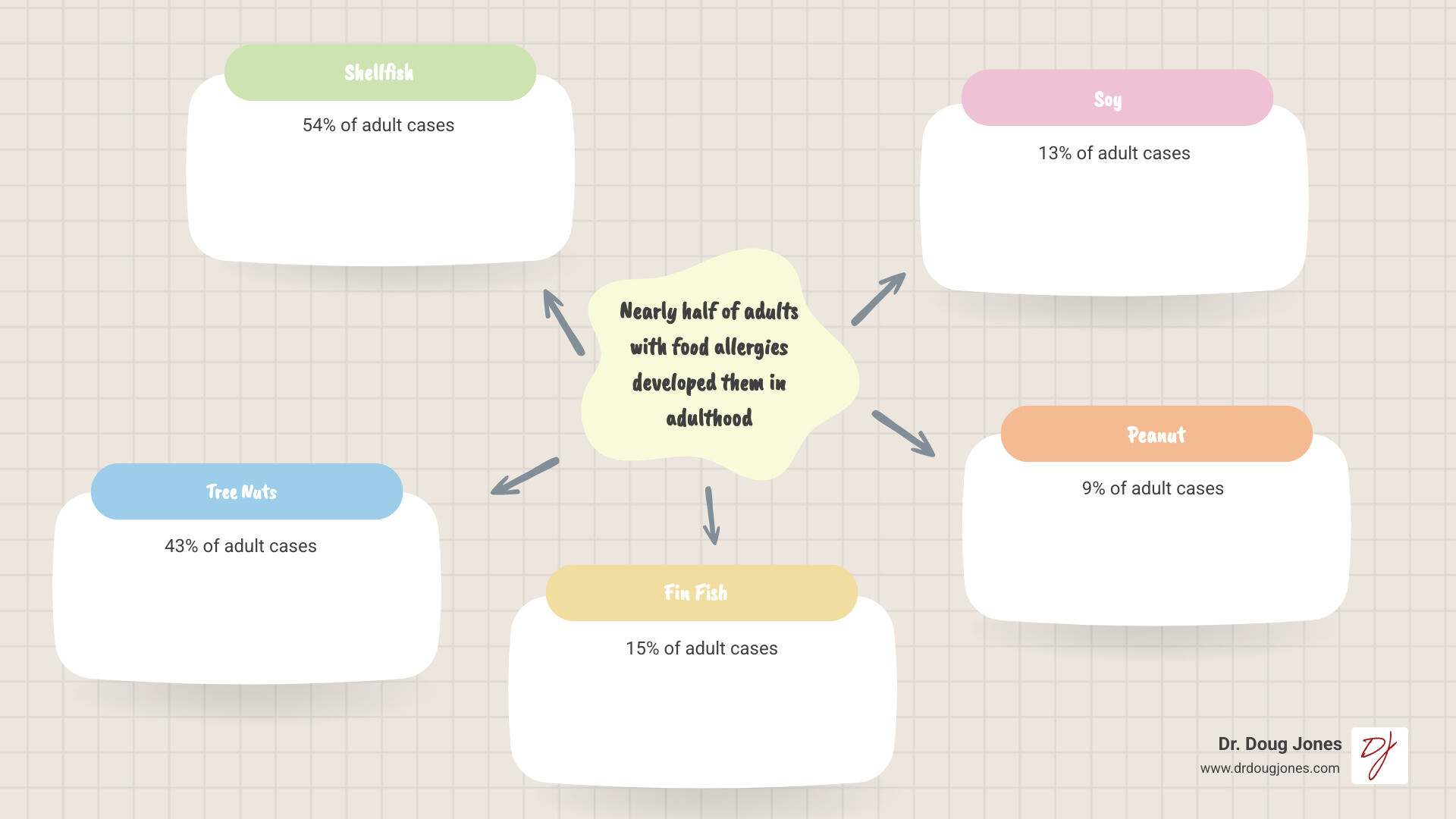
Shellfish tops the list of late-blooming food allergens, accounting for 54% of adult-onset cases in some studies. Following shellfish, tree nuts (43%) and fin fish (15%) are also highly prevalent. Soy (13%) and peanut (9%) also contribute to the adult allergy landscape.
Beyond these, many adults experience Oral Allergy Syndrome (OAS), or Pollen-Food Allergy Syndrome (PFAS). This occurs when the immune system confuses proteins in certain raw fruits, vegetables, or nuts with proteins in pollens (like birch or ragweed). If you have seasonal allergies, you might suddenly get an itchy mouth or scratchy throat after eating a raw apple or carrot. This is a classic example of OAS. While often mild, it can be uncomfortable and, in rare cases, lead to more severe reactions. We've explored this in our article, Why Am I So Itchy With Fresh Fruit and Veggies? Aren't They Supposed to Be Healthy?.
Solving the Causes: Why Do Allergies Develop in Adulthood?
Developing an adult food allergy can feel like a betrayal by your body. This happens because our immune system is not static; it's a dynamic, evolving entity.
Immune system evolution
Our immune system constantly learns and adapts to new pathogens, allergens, and environmental factors throughout our lives. This evolution means new sensitivities, like adult-onset food allergies, can emerge at any time. To learn more, read our guide, Immunity 101: What Your Immune System Actually Does & What People Get Wrong.
While the exact triggers for this immune shift are not fully understood, several factors are believed to play a role:
- Hormonal Shifts: Life stages with significant hormonal changes, such as pregnancy or menopause, may influence immune responses and contribute to new allergies in women.
- Post-Viral Immune Changes: Some evidence suggests that severe infections can alter the immune system, potentially leading to new sensitivities. This is an area of ongoing investigation in immunology.
The Role of Genetics, Environment, and Lifestyle
The complex interplay between genetics, environment, and lifestyle also contributes to adult food allergies.
Genetic Predisposition: A family history of allergies (atopy) increases your risk of developing them later in life, even if you had no childhood allergies. Specific genetic factors have been linked to a compromised skin barrier and an increased risk of developing food allergies. In fact, 67% of adult-onset food allergy patients have a history of other atopic conditions like allergic rhinitis or atopic dermatitis, indicating a broader allergic predisposition.
Environmental Factors: Our surroundings play a crucial role. Changes in geographic location, new environmental allergens, or shifts in our gut microbiome can all influence how our immune system reacts to food. For instance, pollen season in North America has lengthened by 20 days, and pollen concentrations have risen over 20% between 1990 and 2018, which can contribute to food allergies through cross-reactivity.
Cross-Reactivity: As mentioned with Oral Allergy Syndrome, the immune system can confuse similar proteins. If you have a birch pollen allergy, your body might mistakenly react to certain raw fruits or nuts because their proteins resemble those in the pollen.
Alpha-Gal Syndrome: A unique adult-onset food allergy to red meat is Alpha-Gal Syndrome, triggered by a bite from certain ticks, like the Lone Star tick. The tick introduces a sugar molecule called alpha-gal, causing the immune system to produce IgE antibodies against it. Subsequent consumption of red meat can then lead to a delayed allergic reaction. Learn more in our article, When Can a Person Be Allergic to a Sugar? Alpha-Gal Syndrome Explained.
From Symptoms to Diagnosis: Identifying and Confirming an Allergy
When new symptoms arise after eating, it's easy to assume a food allergy, but not every adverse reaction is an allergy.
Differentiating allergy from intolerance
A true food allergy is a potentially life-threatening immune system response where IgE antibodies wrongly identify a food protein as a threat. In contrast, a food intolerance causes digestive symptoms (like bloating or gas) but does not involve the immune system. For example, lactose intolerance is due to a lack of the enzyme lactase, not an immune reaction to milk protein.
Many people mistake intolerance for an allergy. While 11% of U.S. adults have a confirmed food allergy, another 8% report symptoms more consistent with an intolerance. Understanding this distinction is vital for proper management. We dig deeper into this topic in Food Intolerances, Sensitivities, and Allergies: What's the Difference?.
If you suspect an adult food allergy, consult a board-certified allergist. Self-diagnosis can lead to unnecessary dietary restrictions or, more dangerously, prevent you from getting life-saving treatment like epinephrine.
Common Symptoms of Adult Food Allergies
Symptoms of adult food allergies can range from mild to severe and typically appear within minutes to two hours after eating. It's important to recognize how an allergy can manifest:
- Skin Reactions: These are among the most common symptoms.
- Hives (urticaria): Itchy, red, raised welts.
- Angioedema: Swelling, often around the lips, face, or throat.
- Eczema (atopic dermatitis): Worsening of existing rashes.
- Generalized itching.

Gastrointestinal Issues:
- Nausea or vomiting.
- Abdominal pain or cramping.
- Diarrhea.
- Swelling or itching in the mouth or throat.
Respiratory Symptoms: These can indicate a more severe reaction.
- Wheezing or shortness of breath.
- Tightness in the chest or throat.
- Difficulty swallowing or a hoarse voice.
- Nasal congestion or sneezing.
Other Symptoms: A sudden drop in blood pressure, dizziness, or fainting.
In adult-onset cases, skin reactions are frequent, with 73% of patients experiencing them. The most critical concern is the potential for anaphylaxis.
The Dangers of Anaphylaxis
Anaphylaxis is the most severe, life-threatening allergic reaction. It's a rapid, systemic response requiring immediate medical attention. Signs include:
- Respiratory distress: Wheezing, difficulty breathing, throat swelling.
- Cardiovascular symptoms: A sudden drop in blood pressure, dizziness, fainting.
- Skin changes: Widespread hives, flushing.
- Gastrointestinal symptoms: Severe abdominal pain, vomiting.
- Sense of impending doom.
Rising anaphylaxis rates are a serious public health concern. From 2007 to 2016, U.S. insurance claims for food-related anaphylaxis rose 377%. More than a third of these were in adults, who accounted for most claims related to shellfish and food additives. An older age at diagnosis of an adult food allergy is also linked to a higher risk of severe reactions. You can review the FAIR Health data on rising anaphylaxis claims for more.
A biphasic reaction, a second wave of symptoms, can occur hours after the initial anaphylactic event has resolved. This affects up to 20% of cases and underscores the need for medical observation after any severe reaction.
This is why the critical role of epinephrine cannot be overstated. Epinephrine is the first-line treatment for anaphylaxis and must be administered immediately to reverse life-threatening symptoms.
The Path to an Accurate Diagnosis
Given the potential severity of adult food allergies, an accurate diagnosis is paramount. The risks of self-diagnosis are considerable. As many as 1 in 3 people think they have a food allergy, but only about 1 in 28 have a confirmed diagnosis.
The diagnostic process by a board-certified allergist typically involves:
- Medical History: This is the most important tool. Your allergist will ask detailed questions about your symptoms, timing, and suspected foods.
- Physical Examination: A thorough exam helps rule out other conditions.
- Skin Prick Tests (SPT): Small amounts of suspected allergens are pricked onto your skin. A raised, red welt indicates the presence of specific IgE antibodies.
- Blood Tests (Serum IgE): These measure the amount of specific IgE antibodies in your blood.
- Oral Food Challenges (OFC): Considered the gold standard, an OFC involves consuming the suspected allergen under strict medical supervision to definitively confirm or rule out an allergy.
It's vital to rely on these evidence-based methods. For a deeper understanding, refer to our article, Food Allergy Testing 101.
Navigating Life with a New Diagnosis: Treatment and Coping
Receiving an adult food allergy diagnosis can be a jarring experience. The shock of reacting to a lifelong food can be overwhelming, as daily routines like grocery shopping or dining out become potential minefields. It's a profound shift in how you interact with the world.
However, a diagnosis is not an ending but a new beginning—a path to understanding and control. The goal is to empower yourself with knowledge, not live in fear. Our article, Food Allergy Is More Than a Diagnosis: Transitioning From a Life of Fear to Full Food Freedom, explores this transition.
Treatment and Emergency Management
There is no cure for adult food allergies, so management focuses on:
- Strict Allergen Avoidance: This is the cornerstone of management. It means carefully reading ingredient lists and understanding cross-contamination risks.
Epinephrine Auto-Injector: Anyone with a severe food allergy must carry an epinephrine auto-injector (EAI) at all times. This life-saving medication reverses anaphylaxis symptoms. We ensure patients are trained on how to use epinephrine. Soberingly, while 81% of adults with new food allergies require an epinephrine prescription, fewer than 1 in 4 have one. This is a critical safety gap.
Antihistamines for Mild Reactions: For mild, localized symptoms not progressing to anaphylaxis, antihistamines may offer relief. However, they do not treat anaphylaxis and should never replace epinephrine. They are also slow to work. Always discuss their use with your allergist.
For a comprehensive look at options, explore Food Allergy Treatment Options: Finding the Right Fit for You.
Exploring Advanced Treatments Like Oral Immunotherapy (OIT)
While avoidance is fundamental, allergy treatment is advancing. Oral Immunotherapy (OIT) is a promising approach to reduce the risk of severe reactions from accidental exposure.
What is OIT? OIT involves ingesting tiny, gradually increasing doses of the allergen under medical supervision to desensitize the immune system. OIT is a desensitization process, not a cure. It aims to raise the reaction threshold, providing a safety net against accidental ingestion.
How OIT works for adults: While mainly approved for peanut allergy in children, OIT is offered off-label for other allergens and adults by specialists. For those with new adult food allergies, OIT can be a game-changer, reducing sensitivity and anxiety about accidental exposure.
Other advanced treatments include biologic treatments like Omalizumab (Xolair). This anti-IgE medication is approved to reduce allergic reactions, including anaphylaxis, after accidental exposure by blocking the IgE antibodies central to the reaction.
These therapies offer new hope for managing adult food allergies. Learn more in our discussion, A New Era in Food Allergy Treatment: OIT, SLIT, and Biologics Explained.
The Emotional and Social Impact
Living with adult food allergies carries a significant emotional and social burden. Many adults report anxiety and embarrassment, especially when their allergy is seen as an inconvenience.
- Anxiety and Hypervigilance: The constant fear of accidental exposure can lead to chronic anxiety, which can be exhausting and affect quality of life. We explore this in The Emotional Load of Food Allergy: Hypervigilance.
- Navigating Social Events and Dining Out: Social gatherings and dining out can become sources of immense stress, requiring detailed questions about ingredients and constant risk assessment.
- Finding Support Groups: You are not alone. Connecting with others who understand can be incredibly validating. Online groups, like the FAACT Adults with Food Allergies Facebook Page, offer communities for support.
- Personal Stories of Coping: Hearing from others can transform your perspective. Individuals like Felicia Sabartinelli, known as Ms. Allergic to Everything, have openly shared their journeys, reminding us that coping and thriving are possible.
Conclusion: Taking Control of Your Health
The landscape of adult food allergies is complex, but understanding it is the first step toward reclaiming control of your health. We've explored how common these allergies are, their causes, and the critical importance of accurate diagnosis and proactive management.
A diagnosis, while initially daunting, is the first step to safety. It empowers you with the knowledge to avoid triggers, manage reactions, and explore advanced treatments. The journey to managing adult food allergies can be challenging, but with expert guidance, it becomes a clear path forward.
At Dr. Doug Jones's practice, we specialize in offering a new approach to complex immune challenges like adult food allergies. Our commitment is to provide personalized care and education, empowering you with lasting relief and confidence. We believe in working together to understand your unique immune system and equip you with the tools to live a full life. For a personalized approach to your immune health, explore strategies for Immune System Strengthening.
