Breathe Easy: Top Tips for Allergy Symptom Relief
Get comprehensive allergy symptom relief! Discover triggers, meds, natural remedies & lifestyle tips to breathe easy.

Why Effective Allergy Symptom Relief Matters
Allergy symptom relief can transform your daily life, replacing constant sneezing, itchy eyes, and fatigue with comfortable breathing and clear thinking. Whether you face seasonal pollen, dust mites, or food sensitivities, the right strategies can provide immediate comfort and long-term freedom from symptoms.
Quick Relief Options:
- Antihistamines: Block histamine for sneezing, itching, and runny nose (work within 1 hour).
- Nasal corticosteroid sprays: Reduce inflammation and congestion (most effective option).
- Saline nasal irrigation: Flush out allergens and mucus immediately.
- Environmental controls: Use HEPA filters, close windows, and shower after exposure.
- Avoidance strategies: Check pollen counts and time outdoor activities accordingly.
When to Seek Help:
- Symptoms last more than 10 days.
- Medications are ineffective.
- You experience breathing difficulties or throat swelling (call 911).
- Symptoms disrupt sleep or daily life.
Over 50 million Americans experience seasonal allergies annually. The good news is that most allergy symptoms respond well to a structured approach combining trigger avoidance, appropriate medications, and environmental controls.
As Dr. Doug Jones, a board-certified immunologist, I've helped thousands find lasting allergy symptom relief. My practice uses personalized, integrative approaches to address root causes, empowering you to take control of your immune health and break free from chronic allergic reactions.
Understanding Your Allergies: Triggers, Symptoms & Diagnosis
Allergies are your immune system's case of mistaken identity. It treats harmless substances like pollen as dangerous invaders, triggering the release of histamine and causing sneezing, itchy eyes, and a stuffy nose. Effective allergy symptom relief begins with understanding your specific triggers and symptoms.
Common Allergy Triggers and Seasons
Allergic reactions often follow predictable seasonal patterns based on airborne allergens.
- Tree pollen from oak, maple, and birch kicks off the allergy season in early spring.
- Grass pollen takes over in late spring and early summer, often flaring up after lawns are mowed.
- Weed pollen, especially from ragweed, dominates late summer and fall.
- Mold spores thrive in humidity and can be an issue both outdoors and indoors, particularly in damp areas like basements.
Not all allergies are seasonal. Dust mites are year-round indoor allergens found in mattresses, pillows, and furniture. Pet dander (skin flakes, saliva, and urine proteins) from cats, dogs, and other animals is another common year-round trigger.
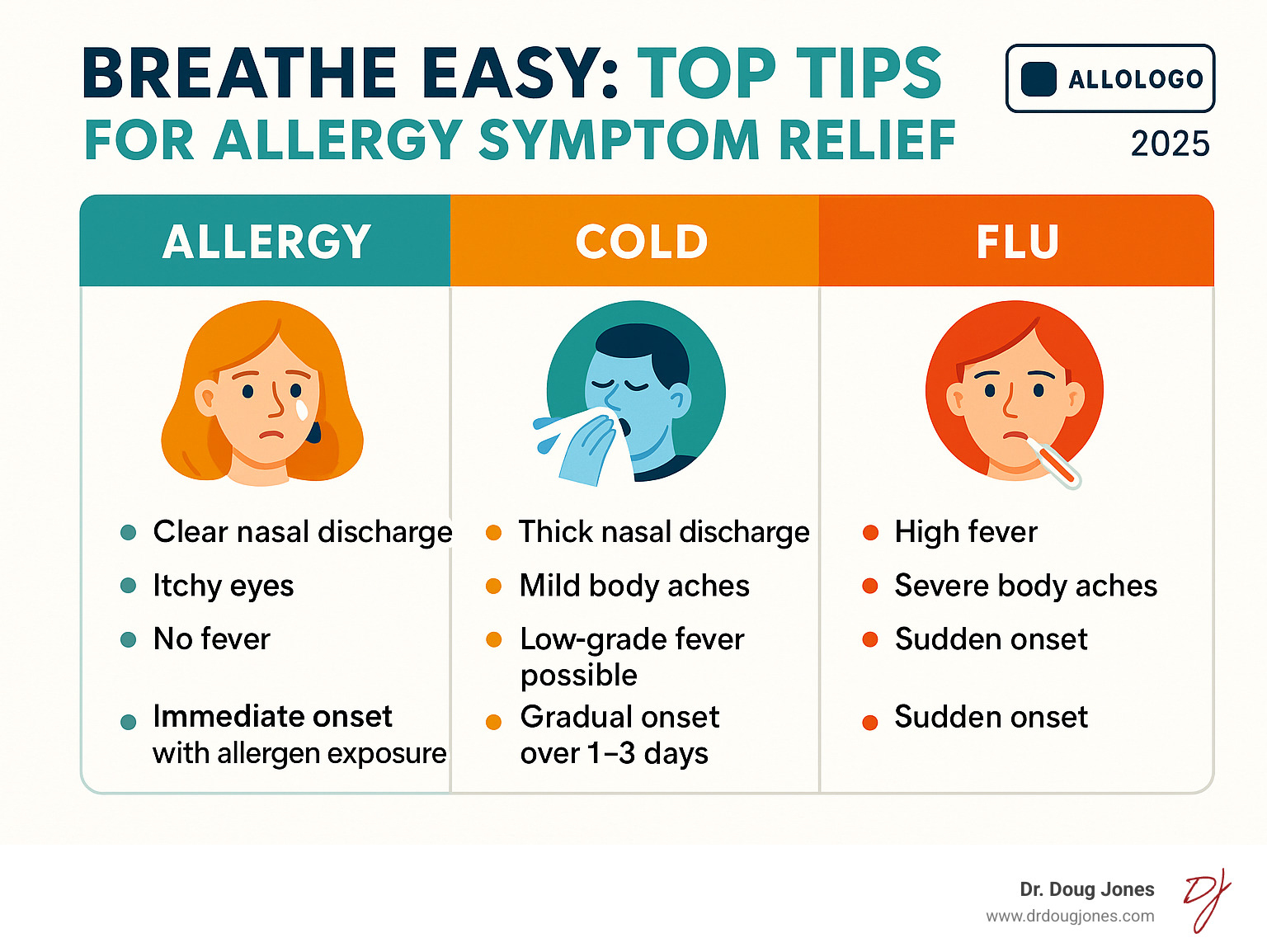
Is It Allergies, a Cold, or the Flu?
Distinguishing between allergies and an infection is key, as treatments differ.
- Allergies: The main giveaway is itching in the eyes, nose, or throat. Symptoms appear immediately upon exposure to a trigger, feature clear, watery nasal discharge, and do not include a fever or body aches.
- Colds: Symptoms develop gradually over 1-3 days and may include thicker, colored mucus, mild body aches, or a low-grade fever. Colds typically resolve in 7-10 days.
- The Flu: Symptoms appear suddenly and are severe, including high fever, significant body aches, and debilitating fatigue.
If you experience the same “sickness” at the same time each year, you likely have seasonal allergies. If symptoms are constant, an indoor trigger is the probable cause.
Pinpointing Your Personal Triggers
Identifying your specific triggers is the most effective step toward allergy symptom relief.
A symptom diary is a powerful tool. Track when and where your symptoms occur and their severity to identify patterns that point to your triggers.
For a definitive answer, allergy testing removes the guesswork.
- Skin prick tests are the gold standard, providing reliable results in about 20 minutes. A tiny amount of an allergen is applied to the skin; a raised bump indicates an allergy.
- Blood tests are an alternative that measures IgE antibodies in your blood to identify reactions to specific allergens.
Your primary care physician can provide an initial evaluation. However, for persistent or severe symptoms, consult an allergist for comprehensive testing and advanced treatment plans, such as immunotherapy.
Lifestyle & Environmental Controls for Allergy Relief
Once you know your triggers, minimizing exposure is the next step. This creates a protective bubble, giving you the freedom to enjoy life without a constant battle for allergy symptom relief.

Managing Outdoor Exposure
Think of managing outdoor allergens as making it harder for them to ruin your day.
- Monitor pollen counts via your local weather forecast and plan activities when counts are low. Pollen typically peaks in the early morning.
- Time outdoor activities for after a good rain, which washes pollen from the air. Avoid being outside on dry, windy days.
- Use protective gear like wraparound sunglasses to shield your eyes and an N95 mask during yard work to filter out pollen.
- Keep windows closed at home and in your car, using air conditioning to stay cool.
Creating an Allergen-Free Haven Indoors
Turn your home into an allergen-free sanctuary with these strategic improvements.
- Use HEPA filters. High-Efficiency Particulate Air filters trap 99.97% of tiny particles like pollen, dust, and dander. Place HEPA air purifiers in bedrooms and use high-efficiency filters (MERV-11 or higher) in your HVAC system.
- Control humidity. Keep indoor humidity between 30% and 50% with air conditioning and dehumidifiers to inhibit mold and dust mites.
- Clean strategically. Vacuum regularly with a HEPA-filter vacuum. Damp mop floors and use wet microfiber cloths for dusting to trap allergens instead of spreading them.
- Protect your bedding. Use allergy-proof covers on mattresses and pillows. Wash all bedding weekly in hot water (130°F+) to kill dust mites.
- Manage pet dander. If you have pets, keep them out of the bedroom, brush them outdoors, and opt for smooth-surfaced furniture like leather over fabric.
Smart Habits for High Pollen Season
Seasonal adjustments can provide significant relief during peak allergy times.
- Dry laundry indoors. Avoid using an outdoor clothesline, as clothes and sheets become pollen magnets.
- Protect yourself during yard work. Wear an N95 mask and eye protection when mowing or raking.
- Shower after outdoor exposure. Immediately rinse allergens from your skin and hair and change clothes to avoid spreading them inside your home.
- Travel smart. Pack your medications, check pollen forecasts for your destination, and request non-smoking, pet-free, or allergy-friendly hotel rooms.
A Guide to Over-the-Counter (OTC) & Prescription Medications
| Medication Type | Symptoms Treated | Onset | Pros | Cons |
|---|---|---|---|---|
| Antihistamines | Sneezing, itching, runny nose, watery eyes | 1-2 hours | Safe for daily use, multiple forms available | May cause mild drowsiness in some people |
| Nasal Steroids | Congestion, inflammation, runny nose, sneezing | 12 hours-2 weeks for full effect | Most effective overall option | Requires consistent daily use, potential for nosebleeds |
| Decongestants | Nasal congestion, stuffiness | 15-30 minutes | Fast-acting relief | Can't use nasal sprays >3 days, not safe for everyone |
When environmental controls aren't enough, medications are your next line of defense for allergy symptom relief. Understanding which tool works best for your symptoms is key.
Antihistamines: Your First Line of Defense
Antihistamines block the histamine that causes sneezing, itching, and a runny nose. Not all are the same. First-generation antihistamines (e.g., diphenhydramine) can cause significant drowsiness and are not recommended for routine use.
Second-generation antihistamines (e.g., cetirizine, loratadine) are the preferred choice for daily use. They are much less likely to cause drowsiness and are effective for long-term relief. Antihistamines are available as pills for systemic relief, as well as nasal sprays and eye drops for targeted symptoms.
For best results, start taking antihistamines daily 2-3 weeks before your allergy season begins. Choose generic versions to save money, as they are chemically identical to brand names. You can also use FSA or HSA funds for these purchases.
Nasal Sprays for Powerful Allergy Symptom Relief
Nasal sprays deliver medication directly to your nasal passages, making them highly effective for nasal symptoms.
- Corticosteroid nasal sprays are the gold standard for allergy relief. They are anti-inflammatory medications that reduce swelling, congestion, sneezing, and a runny nose. For best results, use them consistently, starting 2-3 weeks before allergy season. Aim the spray away from your nasal septum to avoid irritation.
- Mast cell stabilizers (e.g., cromolyn sodium) prevent histamine release. They are very safe but require more frequent dosing and take several days to become fully effective.
Decongestants and Combination Products
Decongestants shrink swollen nasal passages, providing relief from severe blockage. However, they come with important warnings.
- Oral decongestants are not suitable for everyone. Avoid them if you have high blood pressure, heart disease, glaucoma, or an enlarged prostate. They can also interact with certain medications like MAO inhibitors.
- Decongestant nasal sprays provide fast relief but should not be used for more than three consecutive days to avoid rebound congestion, which can be worse than the original stuffiness.
- Combination products blend an antihistamine with a decongestant. Be aware that you are getting the side effects and precautions of both medications.
Safe Allergy Symptom Relief for Special Populations
- Children: Many allergy medications are safe for children (some as young as age 2), but dosing is critical. Always follow age- and weight-specific instructions. Consult a pediatrician if your child needs nasal steroids for more than two months a year.
- Older adults: This group is more susceptible to side effects like confusion or falls from sedating antihistamines. Decongestants can also be problematic. A medication review with a provider is recommended.
- Pregnancy and breastfeeding: Always consult your healthcare provider before taking any allergy medication during pregnancy or while breastfeeding to ensure it is safe for you and your baby.
Natural Remedies & Complementary Therapies
For allergy symptom relief beyond traditional medications, some natural remedies offer valuable, evidence-based support. These approaches work best alongside, not in place of, conventional treatments.

Saline Nasal Irrigation
Saline nasal irrigation is a simple, effective remedy for immediate relief from nasal congestion. It works by washing away allergens and mucus. Clinical trials show it can reduce symptom severity by over 27% and medication needs by over 62%. https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2738432
Water safety is critical. Always use sterile, distilled, or previously boiled (and cooled) water to avoid serious infections. Using a neti pot or squeeze bottle, lean over a sink, tilt your head, and gently pour the solution into your upper nostril, letting it drain from the lower one. Repeat on the other side and clean your device after each use.
Evaluating Herbal and Nutritional Supplements
While many supplements make big promises, only a few have research to back their claims for allergy relief.
- Quercetin: This natural compound may help stabilize histamine-releasing cells. A 2022 study linked quercetin supplements to improved eye and nasal symptoms and better sleep quality. https://www.europeanreview.org/article/29072
- Stinging nettle: This plant has natural anti-inflammatory properties that may help calm allergic reactions.
- Probiotics: Research suggests certain probiotics may help modulate the immune system and reduce allergy symptoms. https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.821900/full
- Vitamin C: Some evidence suggests vitamin C has antihistamine effects. A 2018 study found high-dose intravenous vitamin C reduced allergy symptoms. For daily use, stick to dietary guidelines. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
- Butterbur: Some studies show promise, but ensure any product is labeled "PA-free" to avoid liver toxicity.
Myth Buster: Local Honey. There is no scientific evidence that eating local honey desensitizes you to the tree, grass, and weed pollens that cause most seasonal allergies.
Always discuss supplements with your healthcare provider before use, as natural does not always mean safe.
Are Essential Oils Helpful or Risky?
Essential oils can be helpful but also carry risks. Peppermint oil may decrease nasal inflammation, while eucalyptus oil may help with allergic skin reactions when diluted. https://www.frontiersin.org/journals/allergy/articles/10.3389/falgy.2022.1012183/full
However, essential oils are not regulated by the FDA and can cause skin or respiratory irritation. Always perform a patch test with a diluted oil on a small area of skin first. Never ingest essential oils unless directed by a qualified healthcare professional.
Advanced Strategies and Long-Term Solutions
When daily medications and environmental controls aren't enough, it's time for more targeted, long-term solutions that can retrain your immune system.

Managing Specific Symptoms: Eyes, Skin, and Asthma
- Itchy, watery eyes: Antihistamine eye drops work very well. Pro tip: refrigerate your eye drops for extra soothing relief. Simple cold compresses can also calm inflammation.
- Skin reactions: For localized rashes, topical corticosteroid creams can reduce inflammation and itching. For widespread hives, oral antihistamines provide systemic relief. Seek immediate medical attention for any rash accompanied by facial or throat swelling or difficulty breathing.
- Allergies and asthma: Allergies and asthma are strongly linked, as allergens can trigger airway swelling and tightening. https://www.aafa.org/asthma-symptoms/ If you have asthma, managing your allergies is critical. Always follow your asthma action plan.
Allergen Immunotherapy: A Long-Term Fix
Allergen immunotherapy is the only treatment that addresses the root cause of allergies by retraining your immune system. It's like exposure therapy; by introducing tiny, controlled amounts of an allergen, your body learns to tolerate it.
This approach is for people whose symptoms persist despite other treatments or who want a long-term solution. Immunotherapy is effective for 85% of allergy sufferers, often reducing or eliminating the need for daily medication. https://www.mayoclinic.org/diseases-conditions/hay-fever/symptoms-causes/syc-20373039
- Allergy shots (SCIT): A series of injections given over 3-5 years. After an initial build-up phase, you receive a monthly maintenance dose. https://www.fda.gov/consumers/consumer-updates/know-which-medication-right-your-seasonal-allergies
- Sublingual tablets (SLIT): A needle-free option for dust mite, grass, and ragweed allergies. A tablet is dissolved under the tongue daily at home after the first dose is taken under medical supervision. https://www.fda.gov/consumers/consumer-updates/know-which-medication-right-your-seasonal-allergies
Emergency Situations: Recognizing Anaphylaxis
Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate action. It affects multiple body systems at once.
Signs of Anaphylaxis:
- Skin: Widespread hives, flushing, intense itching.
- Breathing: Wheezing, shortness of breath, chest tightness, swelling of the tongue or throat.
- Cardiovascular: Dizziness, fainting, weak pulse, drop in blood pressure.
- Digestive: Nausea, vomiting, cramps, diarrhea.
- Other: A sudden feeling of impending doom.
What to do: Administer epinephrine immediately and call 911. Antihistamines are not a substitute for epinephrine. Use an epinephrine auto-injector on the mid-outer thigh at the first sign of a severe reaction. Carry two auto-injectors if you are at risk.
Work with your allergist to create an emergency action plan and share it with family, friends, and caregivers. https://www.aafa.org/pollen-allergy/
Frequently Asked Questions about Allergy Relief
Here are answers to the most common questions I hear from patients seeking allergy symptom relief.
What is the fastest way to relieve allergy symptoms?
For the fastest relief, combine multiple strategies:
- Take a non-sedating oral antihistamine (like fexofenadine), which starts working in about an hour.
- Use saline nasal irrigation to immediately flush out allergens and mucus.
- Try a short-term oral decongestant for severe nasal stuffiness.
- Remove yourself from the allergen source: go indoors, close windows, or wear a mask.
For best results, start your daily medications 2-3 weeks before your allergy season begins.
Can you suddenly develop allergies as an adult?
Yes, adult-onset allergies are common. Our immune systems can change throughout life due to new environmental exposures (like moving to a new region), hormonal shifts, or increased stress. It's possible to suddenly react to something you've been exposed to for years without issue. If you develop new, persistent allergy-like symptoms, get tested to identify the trigger.
How can I create a personalized allergy action plan?
A personalized allergy action plan empowers you to manage your health proactively. Work with your doctor or allergist to build your plan:
- Identify Triggers: Use allergy testing and a symptom diary to pinpoint what causes your reactions.
- Establish a Medication Schedule: Plan when to start daily medications based on your allergy season and have emergency treatments (like an epinephrine auto-injector) if needed.
- Define Environmental Controls: List specific actions for your lifestyle, like using HEPA filters or checking pollen counts before outdoor exercise.
- Track Symptoms: Keep notes on your symptoms and the effectiveness of your treatments to help fine-tune your plan.
- Create an Escalation Plan: Know when to call your doctor versus when to see a specialist so you don't suffer unnecessarily.
Take Control of Your Immune Health for Lasting Relief
Finding true allergy symptom relief is achievable. By combining the right strategies, you can move from reactive suffering to proactive management.
The path to lasting relief begins with understanding your specific triggers. Knowing what sets off your immune system—whether it's pollen, dust mites, or pet dander—gives you the power to act.
Avoidance strategies are your first line of defense. Simple changes like using HEPA filters and timing outdoor activities can dramatically reduce your allergen exposure.
When avoidance isn't enough, medication is your ally. From fast-acting antihistamines to powerful nasal sprays, we have effective tools to quiet an overactive immune response.
For a long-term solution, immunotherapy can retrain your immune system to stop overreacting, offering years of freedom from daily symptoms.
Most importantly, personalized care makes all the difference. Your allergies are unique, and your treatment plan should be too.
As a board-certified immunologist, I help patients achieve lasting relief by focusing on the root causes of immune overreactions, not just masking symptoms. My approach is to understand your unique immune challenges and develop a comprehensive strategy to get you back to living fully.
If you're tired of letting allergies control your life, it's time to take a different approach.
Inquire for a personalized consultation and find how targeted, integrative care can help you breathe easier and feel better year-round.
