The Allergy Detective: What to Expect from an Allergic Food Test
Navigate your food allergy journey. Understand symptoms, triggers, and all allergic food test options to get accurate answers.

Why Getting the Right Allergic Food Test Matters for Your Health
An allergic food test is a medical evaluation to identify which foods trigger an immune reaction. For the 32 million Americans with food allergies, accurate testing is crucial. A wrong diagnosis can lead to unnecessary food restrictions or, worse, put you at risk for dangerous reactions.
Many people struggle with mysterious symptoms like chronic hives or digestive issues, but the path to answers isn't always simple. It's vital to distinguish between a true food allergy, which involves the immune system, and food intolerances or sensitivities, which do not. Understanding which tests work—and which don't—can save you time, money, and frustration.
Common Allergic Food Tests:
- Skin Prick Test: Quick results (15-30 min) for immediate reactions.
- Blood Test (Specific IgE): Measures antibody levels, results in 1-2 weeks.
- Oral Food Challenge: The "gold standard" test, done under medical supervision.
- Elimination Diet: Systematically removes and reintroduces foods.
Key Considerations:
- Tests show sensitization, which is not the same as a clinical allergy.
- No test can predict the severity of a reaction.
- Your clinical history is as important as test results.
- A board-certified allergist should always interpret results.
I'm Dr. Doug Jones, a board-certified immunologist. For over a decade, I've helped thousands of patients steer the allergic food test process to find lasting relief from complex immune challenges like food allergies.
Is It a Food Allergy? Understanding Symptoms and Triggers
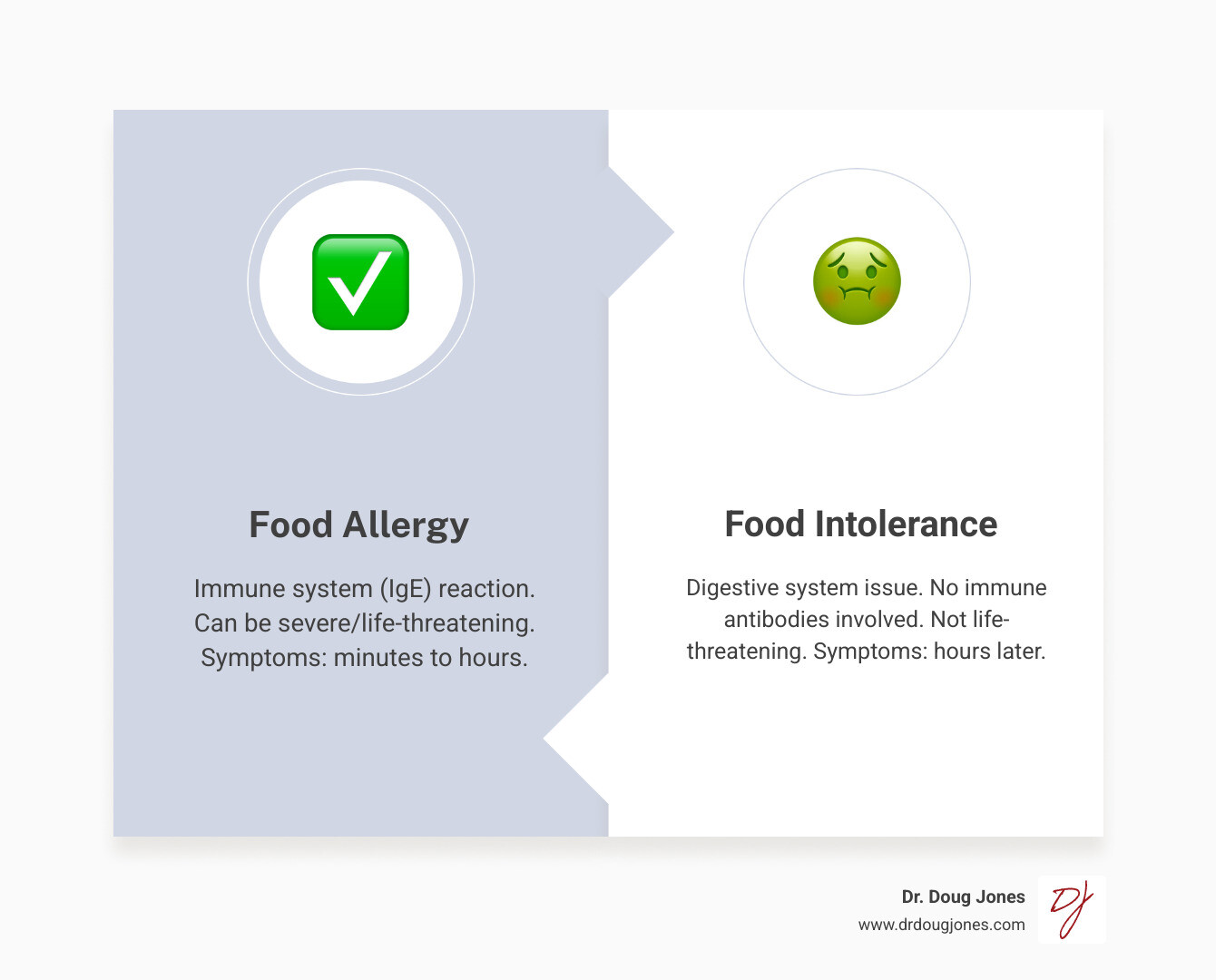
Not all food reactions are created equal. A true food allergy is an immune system error where your body mistakenly identifies a harmless food protein as a threat. It releases IgE antibodies, triggering chemicals like histamine that cause symptoms, which can be life-threatening. Reactions typically occur within minutes to two hours.
In contrast, a food intolerance is a digestive issue, like lactose intolerance, where your body can't break down a food properly. It's uncomfortable but not life-threatening. Food sensitivity is a broader term for milder, often delayed reactions that aren't true allergies or intolerances.
Who Should Consider Food Allergy Testing?
If you experience consistent symptoms after eating certain foods, you may need an allergic food test. Key signs of an immune reaction include:
- Hives: Itchy, raised red bumps appearing within minutes of eating.
- Gastrointestinal Issues: Severe cramps, nausea, vomiting, or diarrhea that occur repeatedly with the same foods.
- Respiratory Symptoms: Shortness of breath, wheezing, a repetitive cough, or a feeling of the throat closing. These are particularly concerning and can escalate quickly.
- Anaphylaxis: A severe, whole-body reaction causing difficulty breathing, dizziness, or a drop in blood pressure. This is a medical emergency requiring an immediate 911 call.
- Oral Allergy Syndrome: Itching in the mouth or swelling of the lips, tongue, or face.
Conditions like moderate-to-severe eczema (especially in children) and eosinophilic esophagitis (EoE) can also be linked to food allergies. Your medical history is a critical piece of the puzzle. We'll discuss your symptoms, timing, family history, and other details to choose the right tests.
The Top 9 Major Food Allergens
About 90% of serious allergic reactions are caused by nine major allergens. U.S. law requires these to be clearly listed on packaged foods, often in a "Contains" statement. Learning to read labels is a crucial skill for managing food allergies.
- Milk: The most common childhood food allergy.
- Eggs: Another common childhood allergy, often outgrown.
- Peanuts: A legume allergy known for causing severe reactions.
- Tree Nuts: Includes almonds, walnuts, cashews, etc.
- Soy: More common in infants and young children.
- Wheat: An immune reaction to wheat proteins, distinct from celiac disease.
- Fish: Often develops in adulthood and is typically lifelong.
- Crustacean Shellfish: The leading cause of food allergies in adults (shrimp, crab, lobster).
- Sesame: The newest major allergen, found in many foods like tahini and breads.
A Comprehensive Guide to Your Allergic Food Test Options
Choosing the right allergic food test depends on your symptoms, age, and medical history. We often use a combination of tests to get the clearest picture of what's happening in your body. The approach may also vary for infants versus adults and for those with coexisting conditions like asthma, eczema, or eosinophilic esophagitis (EoE).
| Test Type | Accuracy (for diagnosis) | Speed | Risk | Preparation |
|---|---|---|---|---|
| Skin Prick Test (SPT) | Indicates sensitization | 15-30 minutes | Mild itching, swelling | Pause antihistamines (5-7 days prior) |
| Blood Test (Specific IgE) | Indicates sensitization | 1-2 weeks for results | Minimal (blood draw) | No specific prep (medications don't typically interfere) |
| Oral Food Challenge (OFC) | Gold Standard (confirmatory) | Hours to a full day | Potential for severe allergic reaction | Pause antihistamines/other meds; avoid suspected food; fasting may be required; medical supervision crucial |
| Elimination Diet | Suggests causality | 1-2 weeks (for elimination) | Nutritional deficiencies if unsupervised | Keep detailed food diary, strict avoidance of suspected foods |
The Skin Prick Test (SPT)
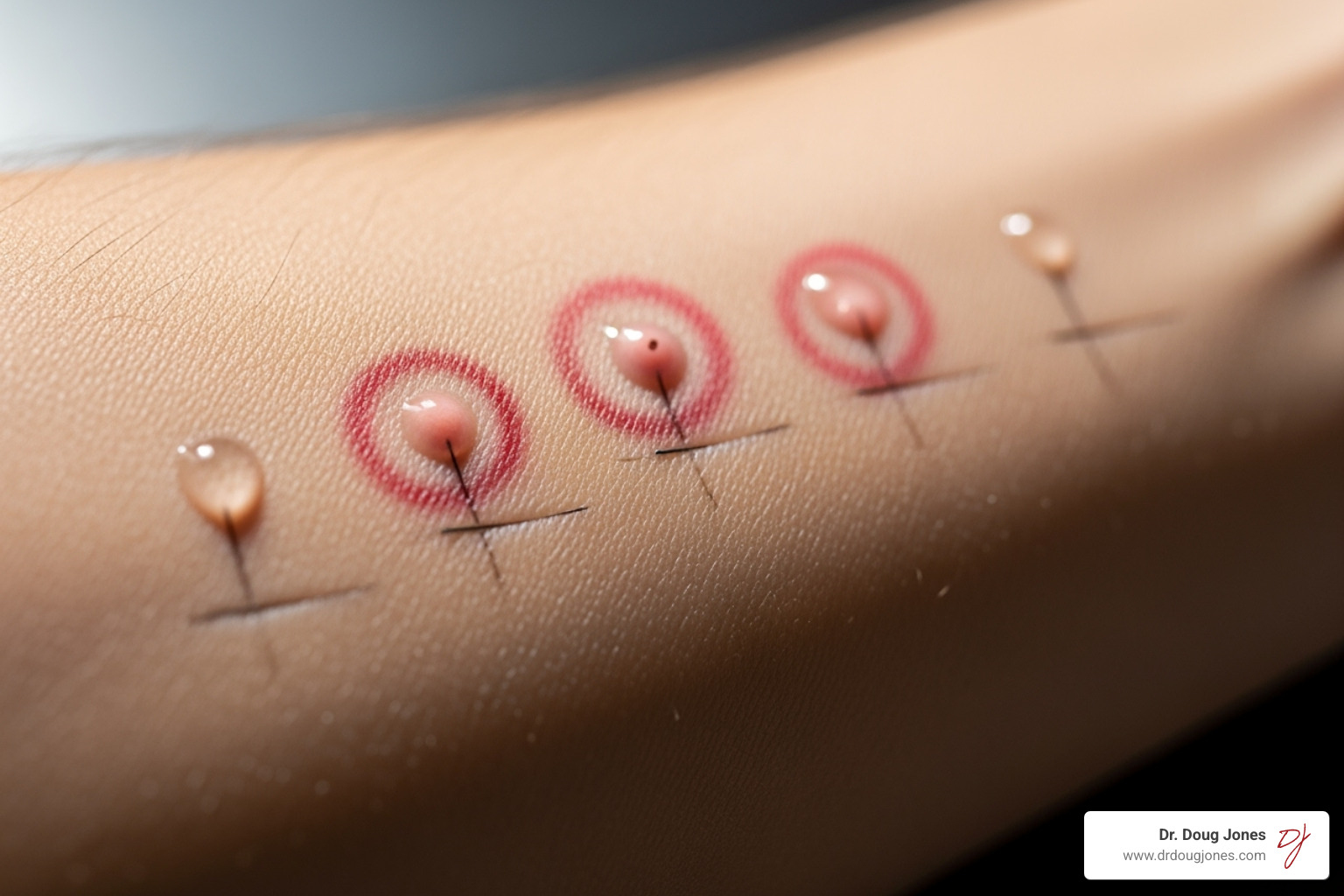
The skin prick test is a fast, common starting point. We place tiny drops of liquid allergen extracts (e.g., peanut, milk) on your arm and gently prick the skin. After 15-30 minutes, we look for a wheal and flare reaction—a raised, red bump like a mosquito bite. A positive result means you are "sensitized" but doesn't guarantee you'll have a clinical reaction. A negative result, however, is highly reliable in ruling out an IgE-mediated allergy. Side effects are typically minor itching at the test site.
The Specific IgE Blood Test: A Common Allergic Food Test
When skin testing isn't an option, a blood test is an excellent alternative. A blood sample is sent to a lab to measure IgE antibodies against specific foods, with results in 1-2 weeks. Like skin tests, a positive blood test shows sensitization versus clinical allergy. Higher antibody levels may suggest a greater likelihood of an allergy, but no test predicts severity. The risks are minimal, and you don't need to stop medications beforehand.

Component-Resolved Diagnostics (CRD)
Component testing is an advanced blood test that goes deeper. Instead of just asking, "Are you allergic to peanuts?" it identifies which specific proteins within the peanut you react to. This helps predict reaction risk and distinguish a true allergy from cross-reactivity. For example, reacting to the Peanut (Ara h 2) protein suggests a higher risk of a severe reaction, while reacting to certain Milk (casein) or Egg (ovomucoid) proteins can predict whether baked forms of those foods might be tolerated.
The Medically Supervised Elimination Diet
When standard tests are negative but symptoms persist, an elimination diet can be useful. This involves removing suspected foods for 1-2 weeks while keeping a detailed symptom diary. If symptoms improve, we guide you through a careful reintroduction phase. This approach is valuable for non-IgE conditions like FPIES and EoE. Medical supervision is crucial to prevent nutritional deficiencies and ensure the process is safe and interpreted correctly.
The Oral Food Challenge (OFC): The Definitive Diagnostic Tool
When we need a definitive answer, we turn to the Oral Food Challenge (OFC). Considered the gold standard, an OFC is the only test that confirms whether eating a food will cause a clinical reaction. We use it to clarify inconclusive test results or to determine if a childhood allergy has been outgrown. Successfully passing an OFC can be life-changing, allowing people to reintroduce foods they've avoided for years.

Safety is our top priority. An OFC is performed in a medical facility equipped to handle any allergic reactions, which are typically mild when they occur. Severe reactions are uncommon when the test is properly supervised. Source
Types of Oral Food Challenges
We choose the type of OFC based on the clinical situation:
- Double-Blind, Placebo-Controlled: The most rigorous method. Neither you nor the medical team knows if you're receiving the allergen or a placebo. This eliminates bias and anxiety from influencing the results. Source
- Single-Blind: You don't know what you're getting, but the medical team does.
- Open-Food: Everyone knows what food is being tested. This is often used when the likelihood of a reaction is low.
During an OFC, you'll eat gradually increasing doses of the food over about an hour, followed by a one- to three-hour observation period. If symptoms appear, the challenge stops, and we provide treatment.
Preparing for Your Allergic Food Test Appointment
Proper preparation is key for accurate results. We will provide specific instructions, but general guidelines include:
- Medications: You may need to pause antihistamines for 3-7 days before a skin test or OFC, as they can block reactions. Talk with your doctor about this first as some may not require this.
- Food Avoidance: For an OFC, you'll need to completely avoid the suspected food for 1-2 weeks prior.
- Fasting: We may ask you to fast for a few hours before certain challenges.
- Time Commitment: Skin and blood tests are quick, but an OFC is a longer appointment, often lasting several hours. Plan accordingly.
After the appointment, we'll discuss follow-up care, whether it's managing a reaction or safely reintroducing a food back into your diet.
Making Sense of Your Results and Planning Next Steps
Receiving your allergic food test results is just one step. A positive skin or blood test means you are sensitized to a food—your immune system has it on its radar. It does not automatically mean you will have a clinical reaction when you eat it. Conversely, a negative test is highly reliable for ruling out an allergy. We never diagnose based on test results alone; your clinical history is essential for proper interpretation. Crucially, no test can predict the severity of a reaction.
Understanding Cross-Reactivity and Oral Allergy Syndrome (OAS)
Sometimes, tests are positive for foods you eat without issue. This may be due to cross-reactivity, where proteins in different substances look similar to your immune system. Oral Allergy Syndrome (OAS) is a common example. If you have a birch pollen allergy, you might get an itchy mouth from raw apples or carrots. If you're allergic to ragweed, raw bananas or melons might cause a similar reaction. These reactions are typically mild, confined to the mouth, and often disappear when the food is cooked, as heat breaks down the problematic proteins.
Creating Your Emergency Action Plan
If an allergic food test confirms a true food allergy, we create a comprehensive safety plan to help you live confidently.

- Strict Avoidance: This involves diligent label reading and learning to spot hidden allergens and cross-contamination risks.
- Epinephrine Auto-Injector: We will prescribe epinephrine and teach you and your family how and when to use it. It is the first-line treatment for severe reactions.
- Anaphylaxis Action Plan: You'll receive a personalized, step-by-step guide that outlines what symptoms to watch for and when to use epinephrine and call 911.
- Education: We help you educate your support network—family, schools, and workplaces—on how to keep you safe. The CDC offers excellent resources for managing allergies in schools.
Long-Term Management and Follow-Up
Managing a food allergy is an ongoing process. We'll discuss if it makes sense to re-test periodically, as some allergies (milk, egg, soy, wheat) are often outgrown in childhood, while others (peanut, tree nuts, fish, shellfish) tend to be lifelong.
Newer desensitization treatments like Oral Immunotherapy (OIT) or Sub-Lingual Immunotherapy (SLIT) can help some patients build tolerance to their allergen under medical supervision. We use ongoing testing to monitor progress and ensure safety. We also help you steer the cost and insurance aspects of testing and treatment. There is also an FDA-approved biologic medication called, omalizumab or Xolair, that can help reduce the risk of reaction upon an accidental exposure. Note, allergenic foods need to be avoided in conjunction with omalizumab usage. Omalizumab can also be used off-label in conjunction with OIT in certain situations. Again, this is something to discuss with your doctor. You are not alone in this; we are your partners in managing your health.
Frequently Asked Questions about Food Allergy Testing
Patients often ask about various allergic food test options they see online. It's important to know what truly helps and what is a waste of time and money.
Are direct-to-consumer and broad screening panels helpful?
Direct-to-consumer (DTC) kits that test for 100+ food sensitivities often cause more harm than good. These panels typically measure IgE antibodies without any clinical context. This leads to a high rate of false positives, causing people to needlessly avoid foods they can safely eat. This can result in nutritional deficiencies and anxiety without identifying the true cause of your symptoms. An allergic food test should always be selected and interpreted by a board-certified allergist based on your specific history. Source
Are hair analysis, bioresonance, or IgG tests valid for food allergies?
No. These methods are not scientifically validated for diagnosing food allergies or intolerances.
- Hair analysis and bioresonance have no scientific basis for detecting immune reactions to food.
- Food-specific IgG tests are particularly misleading. Your body naturally produces IgG antibodies to foods you eat; this indicates exposure, not an allergy or intolerance. A positive IgG test is a normal finding. Relying on these tests often leads to extreme, unnecessary dietary restrictions that can harm your health and quality of life. Source
Stick with proven, evidence-based methods: skin prick tests, specific IgE blood tests, and, when necessary, oral food challenges.
What innovations are changing food allergy diagnosis?
The field is advancing rapidly, moving toward more personalized medicine.
- Component-resolved diagnostics (CRD) are becoming more common, allowing us to pinpoint the specific proteins causing reactions to predict severity better.
- Oral immunotherapy (OIT) and Sub-lingual Immunotherapy (SLIT) offers a path toward desensitization for some patients, with specialized testing used to monitor progress.
- Biologic medications like omalizumab are improving safety and outcomes for desensitization treatments. Source
These innovations allow us to tailor diagnostic and treatment strategies to each person's unique immune profile, offering more precision and hope than ever before.
Conclusion
Navigating the allergic food test can be complex, but you don't have to do it alone. From skin prick tests to oral food challenges, each diagnostic tool offers a piece of the puzzle. The most important takeaway is that testing is a tool, not the final answer. Your symptoms and medical history are just as critical as any lab result.
Understanding the difference between sensitization and a true clinical allergy is key to avoiding unnecessary dietary restrictions and fear. This is why working with a board-certified allergist is essential. We don't just read a report; we listen to your story and create a plan based on the whole picture.
At GAIN, I've seen the life-changing relief that comes from getting accurate answers. No more guessing games or avoiding entire food groups "just in case." Instead, you get a clear action plan, proper emergency preparedness if needed, and the confidence that comes from truly understanding your body.
The field of food allergy is constantly evolving, but the importance of an experienced guide remains the same. We are here to help you make sense of it all and create a personalized plan that works for you.
Ready to get the answers you deserve? Inquire about a consultation to understand your immune health and take the first step toward lasting relief from your food-related concerns.
