The Ultimate Guide to Choosing Your Food Sensitivity Test
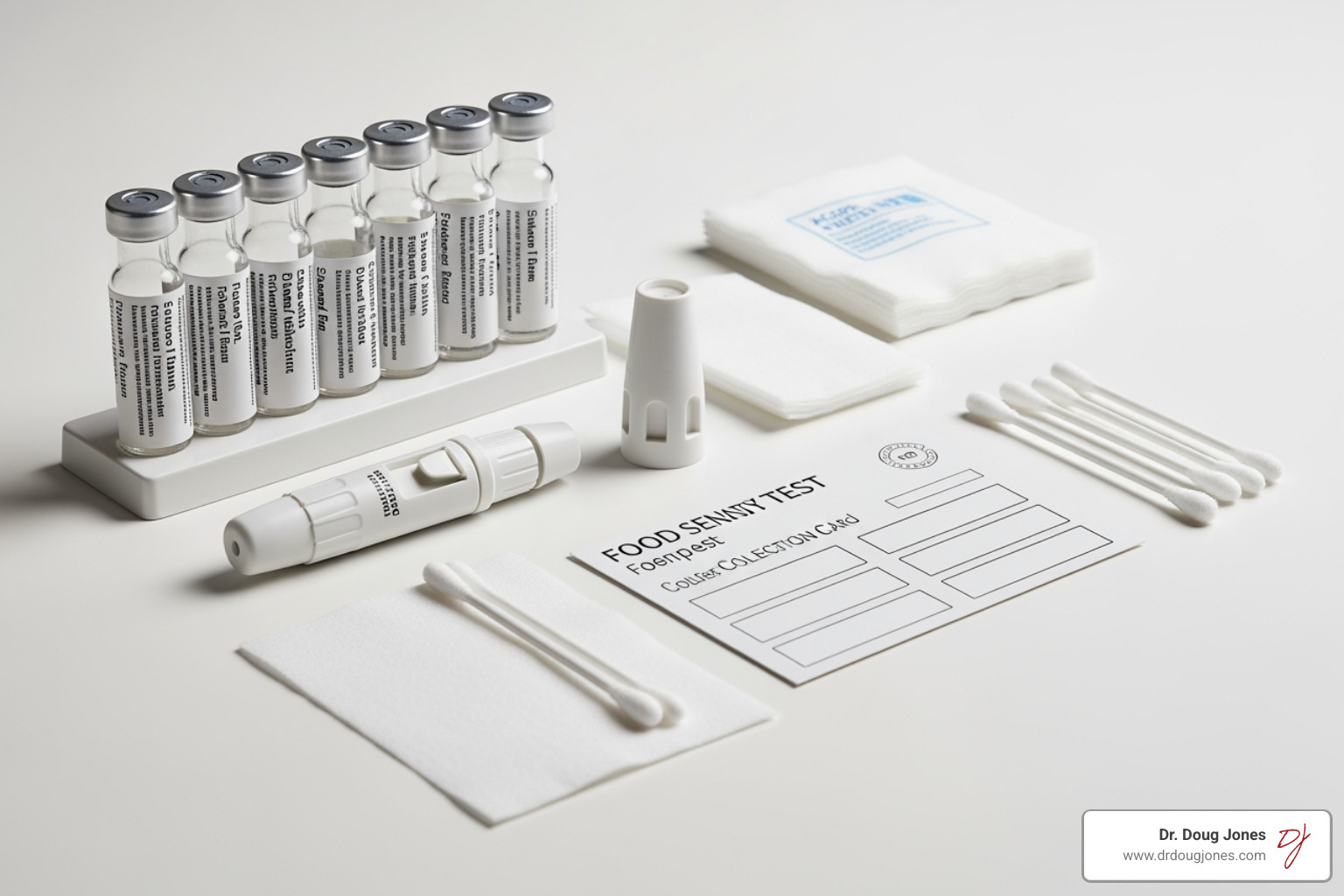
Considering a food sensitivity test? Learn what's real, what's not, and the gold standard for identifying your food triggers. Get informed!
Is It an Allergy, Sensitivity, or Intolerance?
A food sensitivity test can help identify problem foods, but understanding what these tests actually measure—and their limitations—is crucial before you spend your money or restrict your diet.
Quick Answer: Food Test Comparison
- IgE Allergy Tests: Measure immediate immune, IgE-mediated, reactions; validated for true food allergies. Positive tests do not equal allergy, though.
- IgG Food Sensitivity Tests: Limited scientific validation. Do not measure what is often claimed or marketed. No correlation with symptoms have been scientifically established.
- Elimination Diets: Gold standard for identifying trigger foods; requires medical supervision
- Hair/Bioresonance Tests: No scientific evidence; avoid these methods
The confusion around food reactions is understandable. Food allergies involve your immune system and can be life-threatening. Food intolerances are usually enzyme deficiencies (like lactose intolerance) that don't involve immunity. Food sensitivities fall somewhere in between—they may cause real symptoms but the testing methods remain controversial.
Research shows that 32 million Americans have food allergies, while an estimated 10.8% of adults have convincing food allergies. But many more people experience symptoms they attribute to foods—bloating, headaches, fatigue, skin issues—without having true allergies.
The key warning: if you've ever had a severe reaction to food (difficulty breathing, widespread hives, swelling), don't use at-home tests. See an allergist immediately.
As Dr. Doug Jones, a board-certified immunologist with over a decade treating complex immune conditions including food allergies and sensitivities, I've seen how the wrong food sensitivity test can lead to unnecessary dietary restrictions and missed diagnoses. My approach focuses on evidence-based testing combined with comprehensive immune system evaluation to find real answers for lasting relief.
Decoding the Science: What Does a Food Sensitivity Test Actually Measure?
When you're dealing with mysterious symptoms after eating, food testing can feel overwhelming. Let's cut through the confusion and look at what different tests actually measure—and more importantly, which ones you can trust.
Your immune system is incredibly complex, with different types of antibodies doing different jobs. Understanding these biomarkers helps explain why some tests work while others don't.
The Role of IgE in True Food Allergies
IgE antibodies are your body's alarm system for immediate danger. When someone with a true food allergy eats their trigger food, these antibodies spring into action within minutes to a few hours, releasing chemicals like histamine that cause immediate reactions.
The symptoms are hard to miss: hives spreading across your skin, swelling of your face or throat, shortness of breath, vomiting, or dizziness. These reactions can escalate quickly and become life-threatening.
If you've ever experienced severe reactions like difficulty breathing or widespread hives, don't mess around with at-home tests. See an allergist immediately—this isn't the time for DIY diagnosis.
Doctors have reliable tools to diagnose true food allergies. Skin prick testing involves placing tiny amounts of suspected allergens on your skin and watching for raised, red bumps. Blood tests measure specific IgE antibodies in your system. These tests have a high false-positivity rate, so a positive test alone does not diagnose food allergy. Testing needs to be done in the context of the patient and their history. Broad panels of food allergy tests are not recommended, rather targeted testing based on the patient's history. The most definitive test is oral food challenges, where you eat increasing amounts of the suspected food under strict medical supervision with emergency treatment ready by someone with proper experience and training.
Here's something important: if you have asthma, food allergies become even more serious. Asthma is a risk factor for severe or fatal food allergic reactions, making accurate diagnosis crucial.
Some food allergies are particularly tricky. Alpha-gal syndrome causes delayed reactions to red meat—sometimes hours after eating. If you're having mysterious reactions to beef or pork, mention this to your allergist. There are also non-IgE mediated food allergies that can be life-threatening and often elusive to diagnose. An example of this is food protein induced entercolitis syndrome or FPIES. This type of food allergy can also be potentially life-threatening, but presents differently than typical IgE-mediated food allergy as the reactions are often more delayed and gastrointestinal related.
The Controversy Around IgG Food Sensitivity Tests
Now we enter murkier waters. IgG food sensitivity tests are everywhere—from at-home finger-prick kits to fancy lab panels testing dozens or even hundreds of foods. The marketing sounds convincing: high IgG levels supposedly indicate foods causing your bloating, headaches, fatigue, or skin problems because your body is creating an immune response. However, the immune response may not be a bad thing as these antibodies can also confer tolerance to someone. These tests are not validated and do not correlate with clinical symptoms. They should not be used for food allergy, sensitivity, or intolerances. There is limited clinical utility.
But here's where science and marketing clash dramatically.
IgG antibodies are completely different from IgE. They're part of your body's memory system, created when you're exposed to foods regularly. Higher IgG levels don't signal danger—they signal exposure and often tolerance.
Think about it this way: if you eat bread regularly, your body will naturally produce IgG antibodies to wheat. That's normal and healthy, not a sign of sensitivity.
Major medical societies—including the American Academy of Allergy, Asthma & Immunology and the European Academy of Allergy and Clinical Immunology—are crystal clear: IgG and IgG4 food sensitivity tests lack scientific validation for diagnosing food-related conditions.
IgG4 antibodies actually indicate developing tolerance, not sensitivity. They're often liftd in people successfully completing allergy treatments. Using high IgG4 levels to eliminate foods from your diet contradicts basic immunology.
The lack of scientific validation doesn't stop companies from selling these tests. But eliminating foods based on IgG results can lead to unnecessary restrictions, nutritional deficiencies, and missed diagnoses of real medical conditions.
Unvalidated Testing Methods to Approach with Caution
Beyond blood tests, you'll find even stranger options online. Hair analysis claims to identify food sensitivities from a hair sample. Bioresonance testing supposedly detects "energy imbalances" or "vibrational frequencies" related to foods.
These methods have zero scientific basis. Hair doesn't contain the antibodies or immune markers needed to diagnose food reactions. Bioresonance theory contradicts basic physics and biology.
The lack of evidence for these methods is absolute. They're expensive ways to get meaningless results that could lead to misdiagnosis and wasted expense.
Watch for marketing red flags: promises to cure dozens of unrelated symptoms, "secret" technology without scientific explanation, reliance on testimonials instead of research, or tests using hair or saliva for food sensitivities.
The current scientific understanding is clear: reliable food sensitivity testing requires proper immune markers, validated methods, and clinical interpretation. Most commercial food sensitivity tests don't meet these standards.
As someone who's spent over a decade treating complex immune conditions, I've seen too many patients arrive with bags full of supplements and restrictive diets based on unvalidated tests, while their real health issues went unaddressed. The science matters—and so does your health.
The Gold Standard: A Medically Supervised Elimination Diet
Given the limitations of many commercial food sensitivity test options, what's the best approach to identifying food triggers? The gold standard remains a medically supervised elimination and reintroduction diet. This method focuses on your body's direct response to foods, rather than relying on unproven antibody levels or energy readings.
Think of it as detective work—but instead of looking at lab numbers that might not mean much, you're paying attention to how you actually feel when you eat (or don't eat) certain foods. It's more work than ordering a test kit, but it gives you real answers.
The process is straightforward: you carefully remove suspected trigger foods from your diet for a set period, then systematically bring them back one at a time while tracking your symptoms. It sounds simple, but there's an art to doing it safely and effectively.
Safely Navigating an Elimination Diet
Here's the thing about elimination diets—they can be incredibly helpful, but they're not without risks if you go it alone. I've seen too many people restrict their diets so severely that they end up with bigger problems than they started with.
Nutrient deficiencies are a real concern. When you remove entire food groups like dairy, gluten, or multiple fruits and vegetables without proper planning, you might miss out on essential vitamins, minerals, and other nutrients your body needs. This is especially risky for children, pregnant women, or anyone who's breastfeeding.
Disordered eating patterns can develop too. Overly restrictive diets sometimes create anxiety around food, lead to social isolation (ever try going to dinner with friends when you can't eat anything on the menu?), and in some cases, contribute to unhealthy relationships with eating.
Children need special consideration. Eliminating major food groups can affect their growth and development, not to mention turn mealtime into a battleground. Many testing companies won't even offer their services to kids under 18—and there's a good reason for that.
We strongly advise against using direct-to-consumer food sensitivity tests that encourage unsupervised elimination diets, especially if you're dealing with children, pregnant or breastfeeding, have a history of eating disorders, or have ever had severe allergic reactions.
For anyone considering an elimination diet, working with a healthcare provider—ideally an allergist or registered dietitian—is crucial. They can help you weigh the risks and benefits, make sure you're still getting proper nutrition, and guide you through the process safely.
How to Structure Your Elimination and Reintroduction
A safe and effective elimination diet follows a two-part process that requires patience and careful attention to your body's signals.
The elimination phase typically lasts 2-4 weeks. Based on your symptoms and medical history, you'll temporarily remove suspected trigger foods from your diet completely—no cheating, no "just a little bit." During this time, keep a detailed food diary and track your symptoms carefully. You're looking to see if removing these foods leads to improvement.
The reintroduction phase is where the real detective work happens. You'll systematically bring back the eliminated foods one at a time, consuming each for 2-3 days while monitoring for symptoms. Start with small portions and gradually increase them. If symptoms return, you've likely found a trigger. If nothing happens, that food is probably fine to include in your regular diet again.
The one-by-one approach is critical—if you bring back multiple foods at once and have a reaction, you won't know which one caused it.
Working with a dietitian during this process makes a huge difference. They can help ensure you're getting adequate nutrition during elimination and provide strategies for safe reintroduction.
Common trigger foods that often show up in elimination trials include dairy products, gluten-containing grains like wheat, barley, and rye, soy, eggs, corn, peanuts and tree nuts, shellfish, and certain food additives or preservatives. But remember—your trigger foods might be completely different from someone else's.
The beauty of this approach is that it gives you personalized, actionable results based on how you actually respond to foods, not just what a lab test suggests might be a problem.
Could It Be Something Else? Conditions That Mimic Food Sensitivities
Sometimes your body's signals can be confusing. You might think that bloating after lunch or those afternoon headaches are from a food sensitivity, but the real culprit could be something entirely different. This is why jumping straight to a food sensitivity test without considering other possibilities can lead you down the wrong path.
Many medical conditions create symptoms that look and feel exactly like food reactions. The tricky part? Your body doesn't always give you clear clues about what's really going on. That uncomfortable feeling after eating could be your immune system, your digestive enzymes, your gut bacteria, or even your nervous system trying to tell you something.

This gut-brain connection is more powerful than most people realize. Your digestive system has its own nervous system with more nerve cells than your spinal cord. When something's off in your gut, it can affect your mood, energy, and overall well-being in ways that seem completely unrelated to digestion. Learn more about this interplay in the gut–brain axis.
Irritable Bowel Syndrome (IBS) and FODMAPs
If you're dealing with chronic belly pain, bloating, gas, and unpredictable bathroom trips, you might be looking at Irritable Bowel Syndrome (IBS) rather than food sensitivities. IBS affects your gut's normal rhythm and sensitivity, making it overreact to things that wouldn't bother most people.
The interesting thing about IBS is that while certain foods definitely trigger symptoms, it's not usually your immune system causing the problem. Instead, your gut might be extra sensitive to stretching from gas, or your intestinal muscles might not be moving food along properly.
Here's where it gets really specific: many people with IBS find relief with a low-FODMAP diet. FODMAPs are certain types of carbohydrates that can ferment in your gut, creating gas and triggering symptoms. These include things like onions, garlic, certain fruits, beans, and wheat - but not because of gluten.
The FODMAP approach is quite different from eliminating foods based on a food sensitivity test. It focuses on how your gut processes specific types of sugars and fibers, not on immune reactions. This diet is complex and really needs guidance from a dietitian who understands the science behind it.
Getting an IBS diagnosis requires seeing a healthcare provider who can rule out other conditions and look at your specific pattern of symptoms. It's not something you can figure out from a home test kit.
Celiac Disease vs. Non-Celiac Gluten Sensitivity
Let's talk about gluten, because this is where a lot of confusion happens. If you feel terrible after eating bread, pasta, or other wheat products, you might assume you have a gluten sensitivity. But there are actually two very different conditions to consider.
Celiac disease is serious business - it's an autoimmune condition where gluten literally damages your small intestine. When someone with celiac disease eats gluten, their immune system attacks their own intestinal lining. This can cause digestive symptoms, but also fatigue, skin problems, nutrient deficiencies, and even neurological issues.
The key point here: celiac disease requires specific blood tests looking for particular antibodies, followed by an endoscopy to check for intestinal damage. It's a medical diagnosis that needs proper testing.
Non-celiac gluten sensitivity is different. People with this condition feel better when they avoid gluten, but they don't have the autoimmune response or intestinal damage of celiac disease. The diagnosis is usually made by ruling out celiac disease and wheat allergy first, then seeing if symptoms improve on a gluten-free diet.
Here's something really important: a standard IgG food sensitivity test cannot diagnose celiac disease or gluten sensitivity. Celiac is an autoimmune condition that requires specific testing for specific antibodies. Using the wrong test could mean missing a serious medical condition that needs proper management.
Other Common Intolerances
Your body needs specific enzymes to break down different foods. When these enzymes don't work properly, you get symptoms that can look a lot like food sensitivities, but the solution is usually different.
Lactose intolerance is probably the most well-known example. If your body doesn't make enough lactase enzyme, dairy products will cause bloating, gas, and digestive upset. This isn't an immune reaction - it's just missing the right tool for the job.
Histamine intolerance is trickier to spot. Histamine is naturally found in aged cheeses, fermented foods, certain fish, and wine. If your body has trouble breaking down histamine, you might get headaches, skin flushing, hives, or digestive problems. The symptoms can be all over the place, making it easy to mistake for multiple food sensitivities.
Sulfite sensitivity affects some people who react to preservatives in dried fruits, wine, or processed foods. This can trigger asthma symptoms or skin reactions in sensitive individuals.
The challenge with all these conditions is that they can overlap with each other and with true food sensitivities. That's why working with a healthcare professional who understands these different mechanisms is so valuable. They can help you figure out what's really going on instead of guessing based on test results that might not tell the whole story.
Frequently Asked Questions About Food Reaction Testing
I get these questions all the time in my practice, and I understand the confusion around food sensitivity tests. Let me walk you through the most important things you need to know.
What preparation is needed before a food allergy or sensitivity test?
The preparation depends entirely on which type of test you're considering, and honestly, this is where things can get tricky.
For true allergy testing (IgE blood tests), preparation is usually straightforward. You typically don't need to fast or make major changes to your routine. However, if you're taking antihistamines, they might affect skin prick tests—though they usually won't interfere with blood tests. Always discuss your medications with your doctor first.
Here's something that surprises many people: for IgE testing, recent food exposure generally isn't a problem. Your immune system "remembers" allergens whether you ate them yesterday or last month.
IgG food sensitivity tests work differently. Companies often tell you to keep eating the foods you want tested for 4-6 weeks beforehand. Why? Because IgG antibodies reflect exposure—if you haven't eaten something recently, your levels will naturally be low. This actually highlights one of the fundamental problems with these tests: they're measuring exposure, not necessarily sensitivity.
For those unproven hair analysis or bioresonance tests? They claim no preparation is needed because they supposedly measure "energy patterns." But as we've discussed, there's no scientific basis for these methods.
The bottom line: always follow the specific instructions for your test, but more importantly, make sure you're choosing a scientifically validated testing method in the first place.
How accurate are at-home tests and how should I interpret the results?
This is where I see a lot of confusion in my practice. When companies talk about test accuracy, they're often referring to technical accuracy—how well the lab can measure antibody levels. But that's not the same as clinical accuracy—whether those results actually identify foods causing your symptoms.
Many at-home finger-prick food sensitivity tests can accurately measure IgG antibodies. The problem is that high IgG levels often represent normal exposure and tolerance, not a sensitivity that needs treatment. It's like measuring how many times you've shaken hands with someone—it tells you about contact, not whether that person is causing you problems.
This creates a real risk of false positives. You might see high IgG levels to foods you eat regularly and tolerate perfectly well. Following these results could lead you to unnecessarily eliminate healthy foods from your diet.
That's exactly why professional guidance is so important. As an immunologist, I can interpret test results within the context of your complete medical picture. I look at your symptoms, medical history, physical exam findings, and yes, sometimes test results, to piece together what's really going on.
Without this context, test results can be misleading or even harmful. I've seen patients come in after restricting their diets based on unvalidated tests, only to find their symptoms were caused by something entirely different.
When should testing be repeated and how do I adjust my diet long-term?
The decision to repeat any test should always involve your healthcare provider, and the timing depends on your specific situation and the type of test.
For validated IgE allergy testing, we might retest when symptoms change, when we're evaluating whether someone has outgrown an allergy (especially common in children), or when monitoring treatment progress. These decisions are always based on clinical need, not arbitrary timelines.
IgG food sensitivity tests present a different challenge. Given their lack of scientific validation, I generally don't recommend repeating them. Some companies suggest retesting after elimination diets to show "improvement," but this doesn't validate the original test's usefulness. I may utilize them while I am treating an IgE-mediated food allergy to measure their progress and tolerance. These tests should only be utilized by someone who has extensive experience in food allergies.
Here's what I focus on instead: developing tolerance over time. Our immune systems are remarkably adaptable. Sometimes foods that once caused problems can be safely reintroduced later, especially after a period of gut healing and proper treatment of underlying conditions.
The goal is always to eat the widest variety of nutritious foods possible without experiencing symptoms. This isn't about permanent restrictions—it's about finding your personal balance.
I also consider complex reactions like cross-reactivities. For example, if you're allergic to birch pollen, you might react to raw apples or carrots due to similar proteins. These patterns affect both testing interpretation and dietary recommendations.
Long-term success comes from understanding your body's unique responses and working with a knowledgeable healthcare team. We want to solve the underlying issues, not just create lists of foods to avoid forever.
Your Path to Clarity and Relief
After diving deep into food sensitivity tests, blood work, elimination diets, and medical conditions, you might feel a bit overwhelmed. That's completely normal—this is complex territory, and the abundance of conflicting information online doesn't make it any easier.
Here's what matters most: the limitations of many commercial tests are real, and the dangers of misdiagnosis are significant. When you eliminate foods based on unproven test results, you risk creating nutrient deficiencies, developing anxiety around eating, and worst of all, missing an actual medical condition that needs proper treatment.
Think about it this way—if you're spending months avoiding perfectly healthy foods because a hair analysis suggested you're "sensitive" to them, you might be missing the real culprit behind your symptoms. Maybe it's celiac disease that needs proper diagnosis. Maybe it's IBS that could be managed with targeted therapy. Maybe it's a medication side effect or stress-related digestive issues.
What should you do if you've ever had a severe reaction to food? This bears repeating because it's so important: if you've experienced difficulty breathing, widespread hives, or swelling after eating, this is a medical emergency. Call 911 immediately. Don't rely on at-home tests or try to figure it out yourself—anaphylaxis can be life-threatening.
For everyone else dealing with persistent symptoms like bloating, fatigue, skin issues, or digestive discomfort, the value of a comprehensive evaluation cannot be overstated. This means working with healthcare providers who look at your whole picture—your symptoms, medical history, family history, medications, stress levels, and lifestyle factors.
Personalized medicine isn't just a buzzword here—it's about recognizing that your immune system is unique. What triggers symptoms in your friend might be perfectly fine for you. What shows up on a commercial test panel might have nothing to do with how you actually feel after eating certain foods.
My approach focuses on evidence-based testing combined with careful clinical evaluation. We don't just look at isolated antibody levels—we consider how your entire immune system functions, what other conditions might be present, and how different factors in your life might be contributing to your symptoms.
The goal is always to find real answers for lasting relief while avoiding unnecessary restrictions that can harm your relationship with food and your overall nutrition.
If you're struggling with persistent symptoms and suspect food might be playing a role, I encourage you to seek expert help. A board-certified immunologist or registered dietitian who specializes in food reactions can guide you through the process safely and effectively.
Ready to take the next step toward understanding your immune health?

